 The Medical Research Future Fund has announced $15 million in funding for the first Australian – and only the second in the world – clinical trial of mitochondrial donation.
The Medical Research Future Fund has announced $15 million in funding for the first Australian – and only the second in the world – clinical trial of mitochondrial donation.
The new Australian program called mitoHOPE (Healthy Outcomes Pilot and Evaluation) has been established to evaluate the feasibility, safety, and efficacy of mitochondrial donation as a reproductive option.
The program is being led by Monash University and involves a clinical trial that will provide evidence to determine the suitability of mitochondrial donation for clinical practice. The program is also increasing health practitioner knowledge about mitochondrial DNA disease (mtDNA) and providing data to justify its ongoing use in the Australian Health system.
Minister for Health and Aged Care, Mr Mark Butler, made the announcement on 13 March 2023, noting that this is a positive step for all those patients and families who campaigned for Maeve’s Law.
“I’m very pleased to announce $15 million in funding for a mitochondrial donation pilot program,” Minister Butler said.
“Mitochondrial disease is a really challenging condition to navigate. It can be debilitating, with physical and neurological symptoms that are often not fully understood – and there is no cure.
“This funding is about increasing our understanding of the disease so we can better support women and create a brighter future for themselves and their families.”
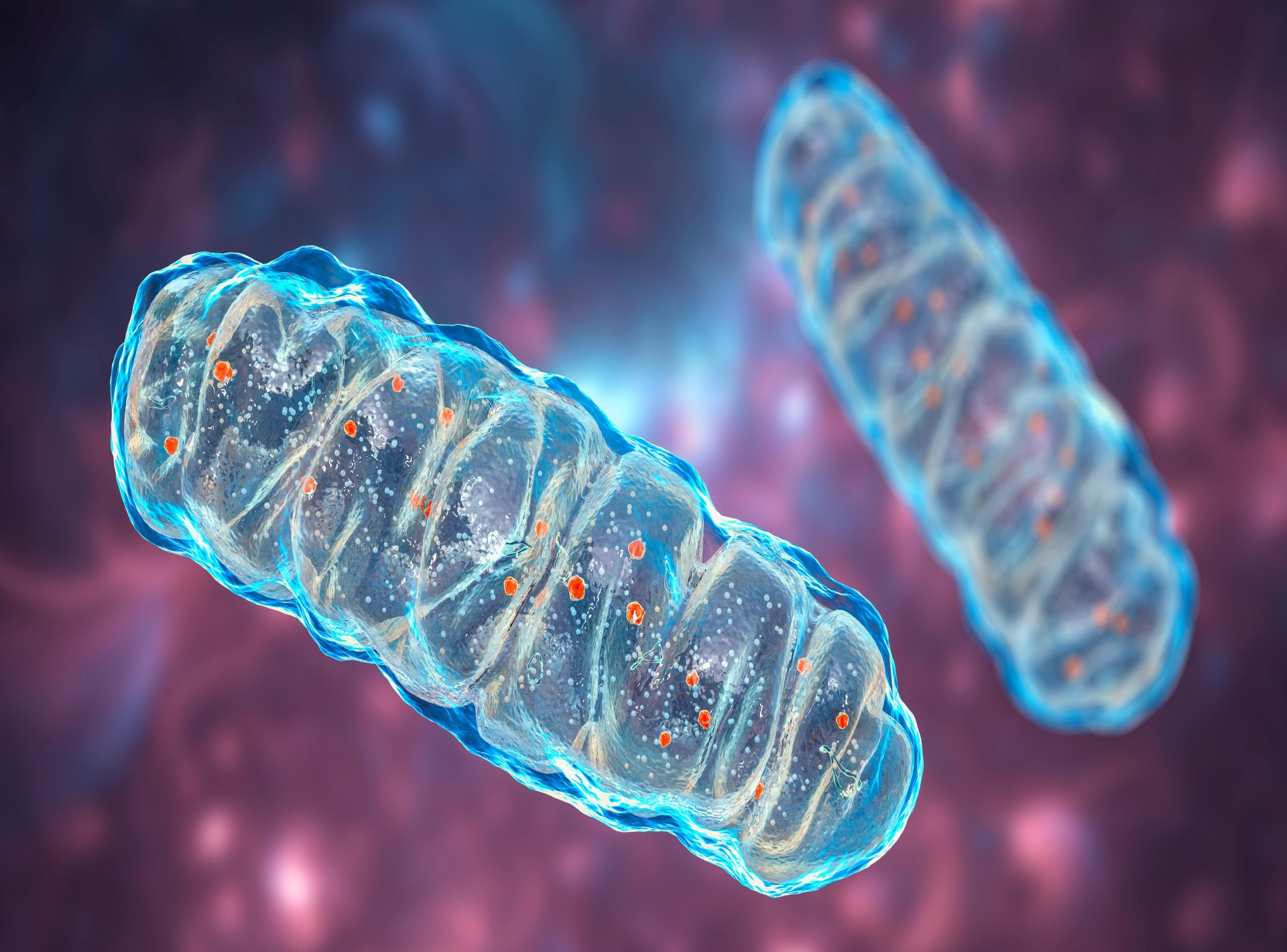
Mitochondria are the power houses of the cell, providing the body with over 90% of the energy it needs to sustain life, and mitochondrial disease (mito) is a debilitating genetic disorder that robs the body’s cells of energy and causes multiple organ dysfunction or failure.
One in 5,000 Australian babies (50 each year) will develop a severely disabling form of mitochondrial abnormalities that can cause death in infancy and childhood, and while current treatments can decrease the impact of symptoms, they do not change the course of the disease – the expected lifespan of these children is only five years.
Mitochondrial donation is an IVF-based technique that has the potential to prevent children from being born with mtDNA.
The technique involves removing the nuclear DNA from a patient’s egg containing faulty mitochondria and inserting it into a healthy donor egg that has had its nuclear DNA removed, ensuring that the unique genetic information that makes an individual who they are and determines what they look like is passed on from mother to child, but the mitochondrial defects are not.
In March 2022, the Australian Parliament passed the Mitochondrial Donation Law Reform (Maeve’s Law) Bill 2021, which established the Mitochondrial Donation Licensing Scheme, which enabled the NHMRC’s Embryo Research Licensing Committee to determine who received a license to use mitochondrial donation.
The Bill provides guidance on who should be considered eligible to use mitochondrial donation, including individuals who are at increased risk of having a child severely affected by mtDNA and for whom other reproductive techniques are unsuitable to reduce this risk.
The mitoHOPE Program will build on this legal foundation and includes mitochondrial and clinical geneticists from Murdoch Children’s Research Institute and around the country, fertility specialists and clinical embryologists from Monash IVF, as well as reproductive scientists from Monash and the University of Adelaide.
The team also includes Monash clinical trial experts and a group of social science researchers to engage with the community, and the consortium will be led by Professor John Carroll, Director of the Monash Biomedicine Discovery Institute (BDI) and an expert in mitochondrial activity in egg and embryo development.
“The entire mitoHOPE team is committed to making this a success for all families who have mitochondrial genetic disease,” Professor Carroll said.
“The Mito Foundation first introduced me to families who have experienced this devastating disease, often over generations, and ever since it has been a priority to ensure we can deliver mitochondrial donation in Australia.”
There are several tasks that need to be completed before at-risk individuals can be admitted to the mitoHOPE clinical trial. These include training embryologists in the laboratory techniques and ensuring that there is a network of health professionals around Australia ready to support families through the program.
However, the most important step is to begin collecting donor eggs from people with healthy mitochondria, which Professor Carroll explained are needed for the mitoHOPE program for two reasons.
“Firstly, donor eggs provide the healthy mitochondria for people undergoing the mitochondrial donation procedure,” she said.
“Secondly, donor eggs are required for the pre-clinical laboratory-based research program, which aims to refine and further validate the mitochondrial donation techniques.”
Professor Catherine Mills, from the Monash Bioethics Centre, who will coordinate the egg donor recruitment programme, pointed out that the success of the MitoHope program will depend on the willingness of Australian women to donate.
“We will be calling on women to consider egg donation for this incredibly important cause,” Professor Mills said.
“Enabling at-risk women to access mitochondrial donation will not only stop the inheritance of mitochondrial genetic disease across generations but also create savings in future healthcare costs of $500 M AUD over 10 years, according to UK health economic studies’ predictions.”
GPs and families can contact the Mito Foundation for information and support.

