CASE 2
19-year-old female experienced a syncopal episode whilst at work and presented to urgent care for further evaluation.
- Patient described sudden onset lightheadedness with blurring of vision then loss of consciousness for seconds before making a full recovery. It occurred after getting up from her desk when walking toward the bathroom.
- History of similar “fainting” spells throughout childhood including during exercise.
- No known family history.
- No regular medications.
- Mild flu like illness last month.
#1. The most consistent diagnosis for this patient:
Results
Correct!
Answer: Long QT Syndrome
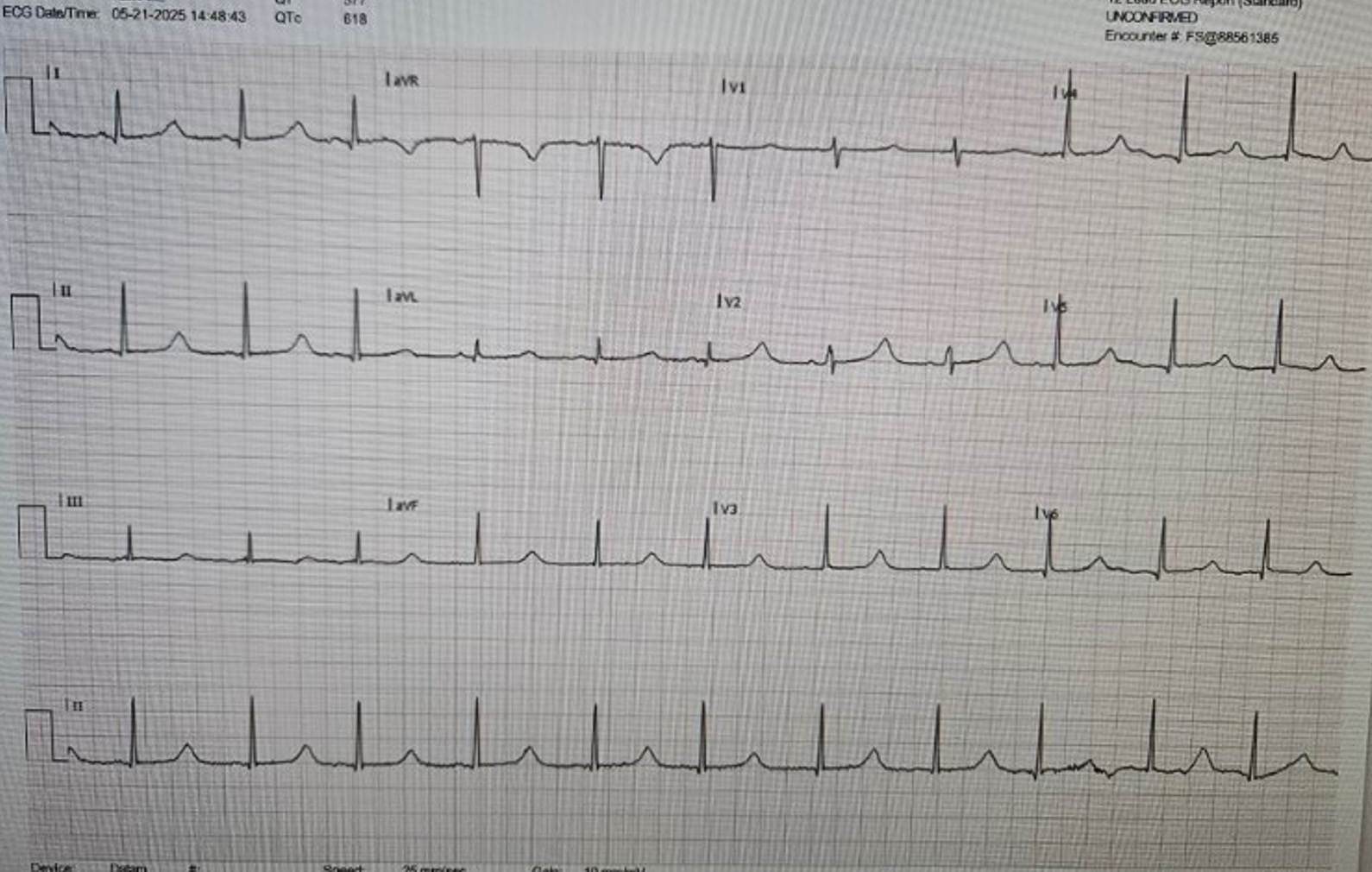
This ECG shows sinus rhythm with a normal PR interval, a normal narrow complex QRS and a very long QT interval. The corrected QT interval is calculated to be 618ms (normal range for female <460ms; males <450ms).
QT interval measurement is best done using the tangent method in leads II and V5. The QT interval need to be corrected for heart rate and although there are many formulae available for this, the most utilised is Bazett’s formula QTc = QT/√(RR).
In the context of the syncopal event and a QTc>500ms it would be appropriate to be concerned about polymorphic VT and a risk of sudden cardiac death. This patient was appropriately admitted to hospital for cardiac monitoring, further evaluation and management.
A prolonged QT can occur in congenital and acquired forms. The acquired form is usually due to drugs, electrolyte abnormalities or other medical conditions (including hypothyroidism, heart failure, intracranial pathology and eating disorders). It is important to take a thorough medication history including illicit drug use.
Congenital long QT syndrome (cLQTS) is a result of genetic mutations affecting ion channels that result in prolonged ventricular repolarisation. The Schwartz score and genetic testing are key tools for diagnosis.
This patient was subsequently diagnosed with congenital long QT 1 with a pathogenic variant diagnosed on gene testing.
Management of cLQTS includes:
- Avoidance of QT prolonging drugs and triggers for all cLQTS patients.
- Beta-blockers (non-selective): Betablockers should be considered for all cLQTS patients. Nadalol has the greatest risk reduction with evidence also supportive of propranolol.
- ICD implantation: There is a clear indication for survivors of cardiac arrest whilst primary prevention requires further consideration and risk stratification.
- Sympathetic denervation.
Wrong answer! Please refresh page and try again