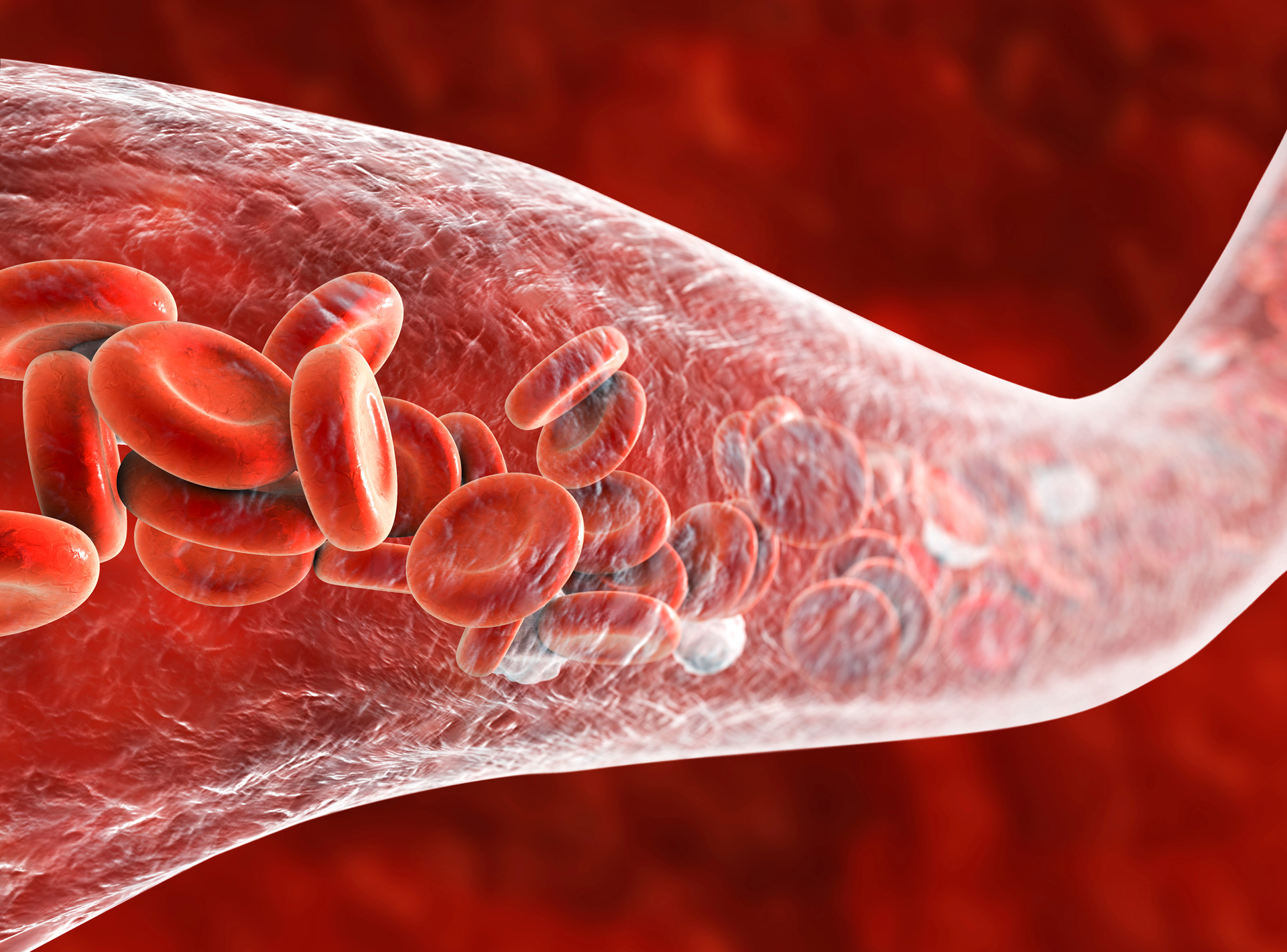
 An international team of researchers led by the University of Sydney report that they have successfully developed a new type of artificial blood vessel, with significant implications for the future of surgery.
An international team of researchers led by the University of Sydney report that they have successfully developed a new type of artificial blood vessel, with significant implications for the future of surgery.
According to the research, published 24 October 2022 in Advanced Materials, preclinical testing found that following transplantation of the manufactured blood vessel into mice, it was accepted by the body, with new cells and tissue growing in the right places, transforming the implant into a ‘living blood vessel.’
Compromised arteries can result in myocardial infarction – the leading cause of death worldwide – and when required, an autologous vascular graft can be used to repair the damaged artery.
Grafts harvested from the saphenous veins, radial arteries, and internal mammary arteries of patients have been considered the gold-standard, yet for patients with limited capacity due to pre-existing pathological conditions, access to off-the-shelf synthetic grafts would provide alternative surgical options.
Senior author Professor Anthony Weiss, from the Charles Perkins Centre, explained that while autologous arteries contain a distinctive intima-media composed of organized elastin and an adventitia containing mature collagen fibrils, in contrast, implanted biodegradable small-diameter vascular grafts do not present spatially regenerated, organized elastin.
“[This] prevents the appropriate arrangement of SMCs and endothelial cells, jeopardizing the graft’s long-term performance,” Professor Weiss said.
“While others have tried to build blood vessels with various degrees of success before, this is the first-time scientists have seen the vessels develop with such a high degree of similarity to the complex structure of naturally occurring blood vessels – nature converts this manufactured tube over time to one that looks, behaves, and functions like a real blood vessel.”
The elastin-containing structures within the intima-media region encompass the elastic lamellae (EL) and internal elastic lamina (IEL) and are crucial for normal arterial functions, such as conveying elasticity for vessel deformation during blood pressure changes and regulating arterial SMC phenotype in response to injury.
“The technology’s ability to recreate the complex structure of biological tissues shows it has the potential to not only manufacture blood vessels to assist in surgery, but also sets the scene for the future creation of other synthetic tissues such as heart valves,” Professor Weiss said.
“The results shown here demonstrate for the first time that we are aware of, the generation of a neo-artery, from an implanted vascular graft, that recapitulates the native artery with respect to the content and spatial distribution of both collagen and organized elastic lamellae (EL).”
Traditionally, the use of porous grafts in vascular settings has permitted the uncontrolled migration and infiltration of fibroblasts and arterial smooth muscle cells (SMCs) from adjacent native tissue into the implanted graft to synthesize an extracellular matrix (ECM), in chaotic competition with infiltrating phagocyte-like macrophages that attempt to degrade the graft.
“This results in the random deposition of collagen and elastin within the graft pores, and we propose that the graft then serves as a physical barrier that prevents the deposited amorphous elastin from connecting and organizing into EL,” Professor Weiss explained.
“There was an unmet demand for structural resemblance to the adjoining native artery, namely highly organized concentric layers of elastin alternating with SMC layers in the media, and hierarchically arranged collagen fibres in the adventitia.”
Lead author and bioengineer Dr Ziyu Wang, also from the University of Sydney’s Charles Perkins Centre pioneered the technology as part of his PhD, building on earlier work by his colleague at the Centre, Dr Suzanne Mithieux.
“These synthetic vessels are elegant because they are manufactured from just two naturally occurring materials that are well-tolerated by the body,” Dr Wang said.
“Tropoelastin (the natural building block for elastin) is packaged in an elastic sheath which dissipates gradually and promotes the formation of highly organised, natural mimics of functioning blood vessels.”
“After implantation in a mouse’s abdominal aorta, the graft develops distinct cell and extracellular matrix profiles that approximate the native adventitia and intima-media by 8 weeks, and within the newly formed intima-media region there are circumferentially aligned smooth muscle cell layers that alternate with multiple EL like that found in the arterial wall.
“By 8 months, the developed adventitia region contains mature collagen fibrils, and the neo-artery presents a distinct IEL with thickness comparable to the rest of the abdominal aorta.”
The manufactured tube can also be safely stored in a sterile plastic bag until transplantation.
Co-author Dr Christopher Breuer, from the US Centre for Regenerative Medicine at Nationwide Children’s Hospital, said he was excited about the potential of the research for children.
“Currently when kids suffer from an abnormal vessel, surgeons have no choice but to use synthetic vessels that function well for a short time but inevitably children need additional surgeries as they grow,” Dr Breuer said.
“This new technology provides the exciting foundation for the manufactured blood vessels that to continue to grow and develop overtime.”

