 A 3-month-old boy presented to our clinic with several well-defined erythematous and annular plaques with indurated borders located on the face appearing 3 weeks post-partum.
A 3-month-old boy presented to our clinic with several well-defined erythematous and annular plaques with indurated borders located on the face appearing 3 weeks post-partum.
Initial Presentation: A baby with red plaques on the face
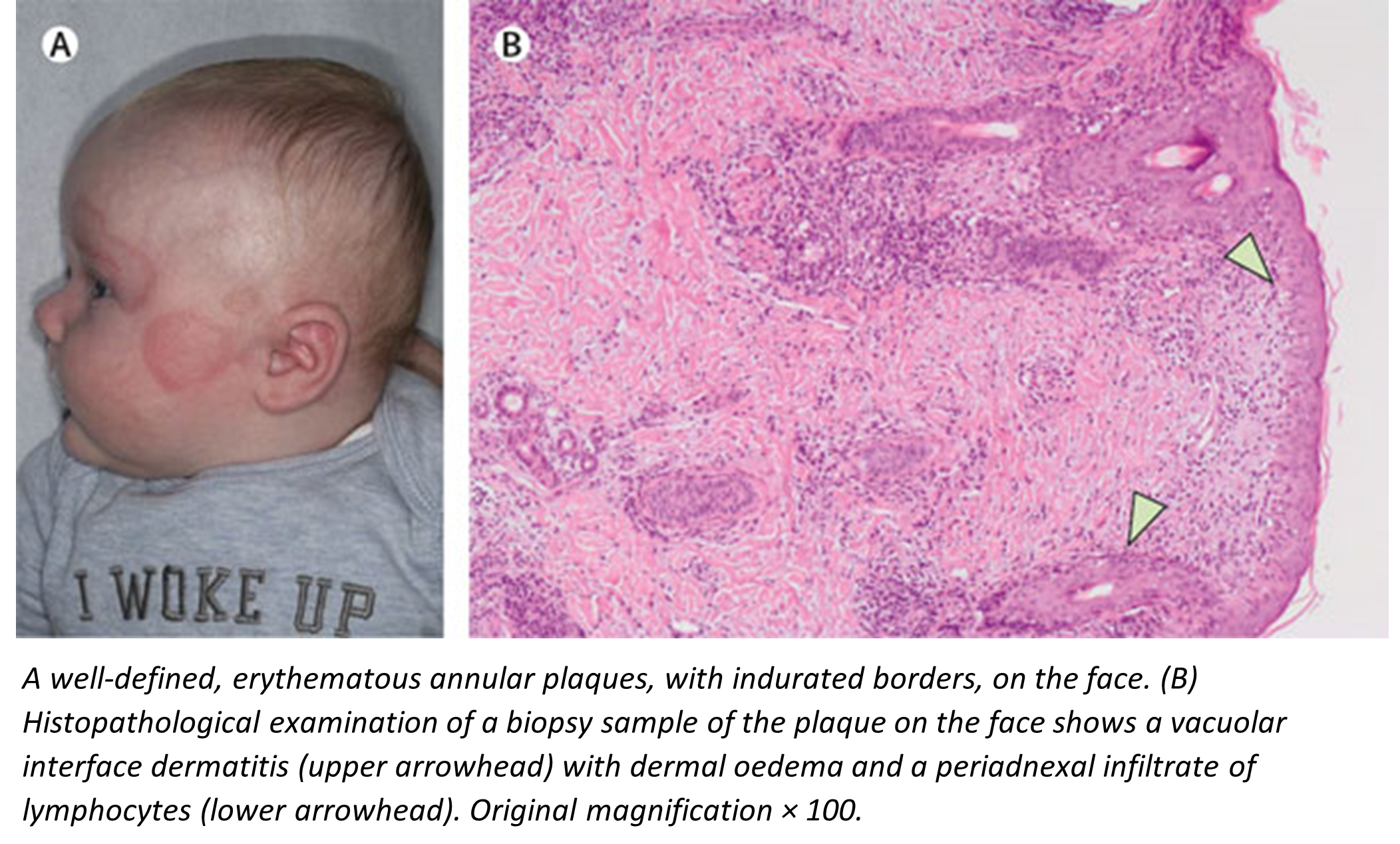
Description: A 3-month-old boy presented to our clinic with several well-defined erythematous and annular plaques with indurated borders located on the face appearing 3 weeks post-partum. Histological examination showed a vacuolar interface dermatitis with dermal oedema and periadnexal infiltrate of lymphocytes.
Need more information?
The 3-month-old boy was brought by his mother to our clinic who had noticed that her child had developed several round red lesions on his face (figure). She said that the problem had begun 3 weeks post-partum. The baby had been born at full term following an uncomplicated pregnancy. The patient’s mother was fit and well, with no medical history of note—specifically she did not report any previous infections, or dermatological or autoimmune diseases.
What is the most likely diagnosis?
- Sweet syndrome
- Atopic eczema
- Neonatal lupus erythematosus
- Cutaneous sarcoidosis
Answer: Neonatal lupus erythematosus
Breakdown: The baby had been seen by another dermatologist when he was 10 weeks old and given topical antifungal treatment—miconazole cream—and a low potency topical corticosteroid cream—hydrocortisone—which had no effect after a 2-week trial.
On examination, we found six, well defined, erythematous annular plaques, with indurated borders, on the baby’s face. We found no other abnormalities: the baby’s temperature was normal, his heart rate was 138 beats per min, and the respiratory rate was 36 breaths per min.
Histopathological examination of a biopsy sample of the plaque on the face showed a vacuolar interface dermatitis with dermal oedema and a periadnexal infiltrate of lymphocytes (figure). Laboratory blood tests showed that both the mother and child were positive for antibodies against extractable nuclear antigen. They were also positive for anti-Sjögren’s syndrome type A (SSA) and anti-Sjögren’s syndrome type B (SSB) antibodies. The erythrocyte sedimentation rate was 11 mm per h, the C-reactive protein concentration was 0·6 mg/L. The white cell count was 13·85 × 109 per L—the neutrophil count was 1·47 × 109 per L, eosinophils 0·18 × 109 per L, basophils 0·02 × 109 per L, lymphocytes 10·58 × 109 per L, and monocytes 1·60 × 109 per L. Both liver and kidney function tests were normal.
Taken together with the findings of the biopsy, we diagnosed neonatal lupus erythematosus.
Given that heart abnormalities are associated with the condition, we referred the baby to a paediatric cardiologist who requested an electrocardiogram which showed findings consistent with first-degree atrioventricular block.
3 months later at a follow-up appointment, all the baby’s skin lesions had resolved without any scarring.
Finally, again given the diagnosis and the positive antinuclear antibodies, we referred the patient’s mother to a rheumatologist who diagnosed Sjögren’s syndrome.
Neonatal lupus erythematosus is a passively acquired, self-limiting, autoimmune disease thought to be caused by the transplacental passage of anti-SSA and anti-SSB antibodies from mother to fetus: the skin—and more importantly—the heart are particularly affected. In approximately half the cases, the mothers are asymptomatic at time of presentation. The cutaneous manifestations in the baby usually develop within the first few weeks of life—typically appearing on the scalp and periorbital areas. The association of the skin lesions with positive anti-SSA and anti-SSB tests in both mother and baby is well recognised, and a skin biopsy is not necessarily required to make the diagnosis. The important complication of congenital heart block—which usually develops in utero and generally resolves—is rare and found in approximately 2% of pregnant women with anti-SSA or anti-SSB antibodies. The skin manifestations in neonatal lupus spontaneously resolve after 4–6 months.
Source: All content for this “Diagnostic Puzzle” was sourced from The Lancet. The article was written by Sayed Meelad Habib, PhD, and Prof Maarten H Vermeer, MD, both from from Leiden University Medical Center, Leiden 2333 ZA, Netherlands.
Original article is available at:
https://www.thelancet.com/doi/story/10.1016/pic.2020.10.30.108552
and
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)32176-0/fulltext
For more Diagnostic puzzles, go to: Picture Quiz Gallery (thelancet.com)

