 ED: 75% of hospital readmission’s are due to medication errors. In older people, I wonder how many are these drugs and HF.
ED: 75% of hospital readmission’s are due to medication errors. In older people, I wonder how many are these drugs and HF.
One challenges of looking after heart failure (HF) patients is managing their pharmacotherapy: at least 40% have five or more chronic conditions. This leads to the average HF patient taking 6.8 medications per day, not including over the counter and complimentary medicines. Getting drugs right on guideline-mandated therapy is one thing but we have to avoid getting them wrong too, avoiding any that cause unacceptable side effects in patients.
These drugs for avoidance in general practice, is not meant to be all inclusive.
Non-steroidal drugs and Cox-2 inhibitors

These are obvious. Prostaglandin inhibition leads to sodium and water retention and blunted response to diuretics. Observational studies support a risk of HF precipitation or exacerbation.
Central acting calcium channel blockers
Verapamil and Cardizem have the strongest negatively inotropic effects and are contraindicated. Dihydropyridones such as nifedipine and (less so) amlodipine have also been linked to worsening heart failure.
Moxonidine
This one is somewhat counter intuitive, as this drug reduces sympathetic outflow. However, a trial in HF patients showed that Moxonidine increased mortality.
Minoxidil
A different drug, a vasodilator; in HF patients it increased LVEF but also increased clinical events (worsening HF, death).
Biguanides
Metformin is safe in stable HF patients with preserved renal function (eGFR >60ml/min) but should be avoided in unstable or hospitalized patients with HF. The concern is over lactic acidosis.
Thiazolidinediones aka “glitazones”
These cause sodium and water retention, generally increasing the risk of worsening HF and hospitalisation. They are best avoided in HF patients, particularly with any symptomatic HF (NYHA II or above)
Dipeptidyl Peptidase-4 Inhibitors aka “gliptins”
Saxagliptin, in particular, in a large trial was associated with an excess of HF hospitalisation. Meta-analysis of all randomized trials of these types of agents has shown an increase in risk of HF. A trial of alogliptin showed a non-significant increase in hospital admission rates for HF but the previous meta-analysis suggests a possible class effect. The exact mechanism is unknown.
Cilostazol
In patients with peripheral vascular disease increases walking distance but inhibits phosphodiesterase type 3 and is believed to increase fatal arrhythmia risk. It remains contraindicated in HF.
Inhaled Beta-agonists
Evidence of a worsening of heart failure is limited to small trials and is not homogenous. However, there is a proposed mechanism of receptor responsiveness with regular use and HF deterioration. Australian HF guidelines recommend minimising exposure to these, and favouring antimuscarinic agents.
Decongestants etc
Prolonged, excessive use of phenylephrine and pseudo ephedrine should be avoided as these drugs act on adrenergic receptors to exert their vasoconstrictive effect.
Tumour necrosis factor-alpha inhibitors
Etanercept seemed to have no negative impact on HF patients. Infliximab had higher rates of HF hospitalisation or death in NYHA class III or IV patients. These drugs are contraindicated in moderate to severe HF and are used cautiously in milder cases.
Anagrelide
Used to decrease the platelet count in myeloproliferative disorders, this drug inhibits phosphodiesterase similarly to milrinone and can cause a high output HF syndrome.
Stimulants
A popular choice in my public outpatient clinic, drugs such as dextroamphetamine and methamphetamine are linked with reports of sudden death, myocardial infarct etc.
Pregabalin
This can cause a peripheral oedema effect, probably via a similar mechanism to nifedipine.
Clozapine
Causes myocarditis, perhaps through an IgE mediated hypersensitivity; incidence about 1% over 10 years.
Complimentary/Alternative Medicines (CAMs)
Frequently used despite guidelines suggesting they not be, and have no role in HF management. Ephedra like compounds (Ma-haung) should be avoided because of their stimulant effects. CAMs can interact negatively with mainstream drugs. A useful table of interactions is below.
Table: CAMs drug interactions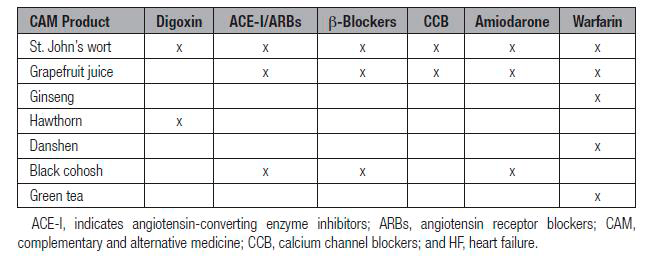 References available on request.
References available on request.
Questions? Contact the editor.
Author competing interests: nil relevant disclosures.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

