CASE 3
16-year-old female with Vietnamese background, developed palpitations and light-headedness during a dance lesson at school. After symptoms did not resolve, her mother brought her to the emergency department at the local regional hospital.
- Background history of exercise induced palpitations for many years that usually resolve within minutes of the cessation of exercise. No history of syncope.
- Episodes of resting palpitations that feel fast and regular intermittently over prior 12 months.
- No known family history of cardiac conditions or sudden death.
- Afebrile, hypotensive and tachycardic on examination.
#1. The most consistent diagnosis for this patient is:
Results
Correct!
Answer: Pre-excited atrial fibrillation
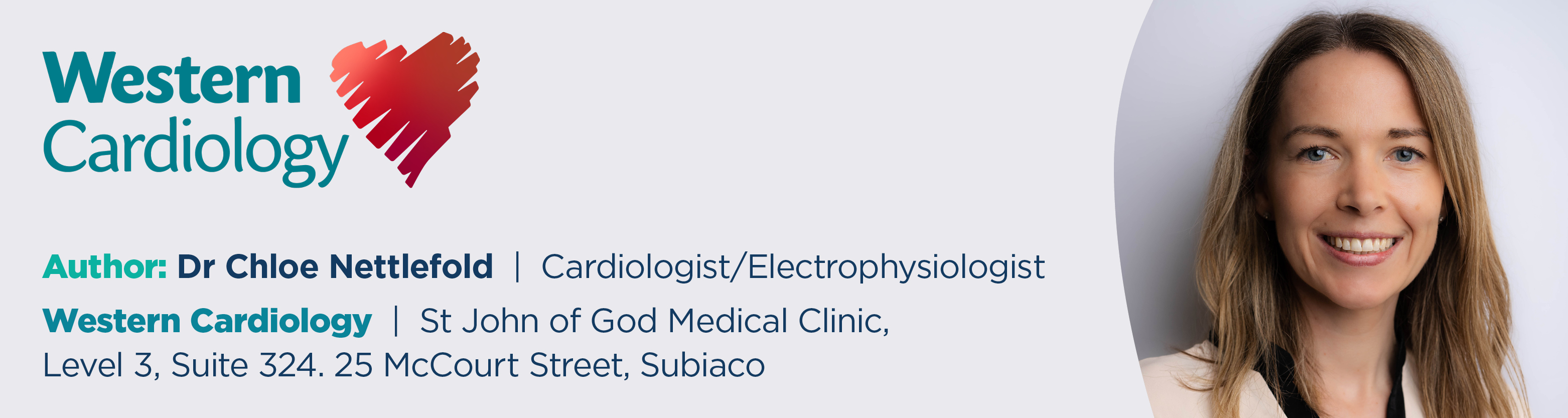
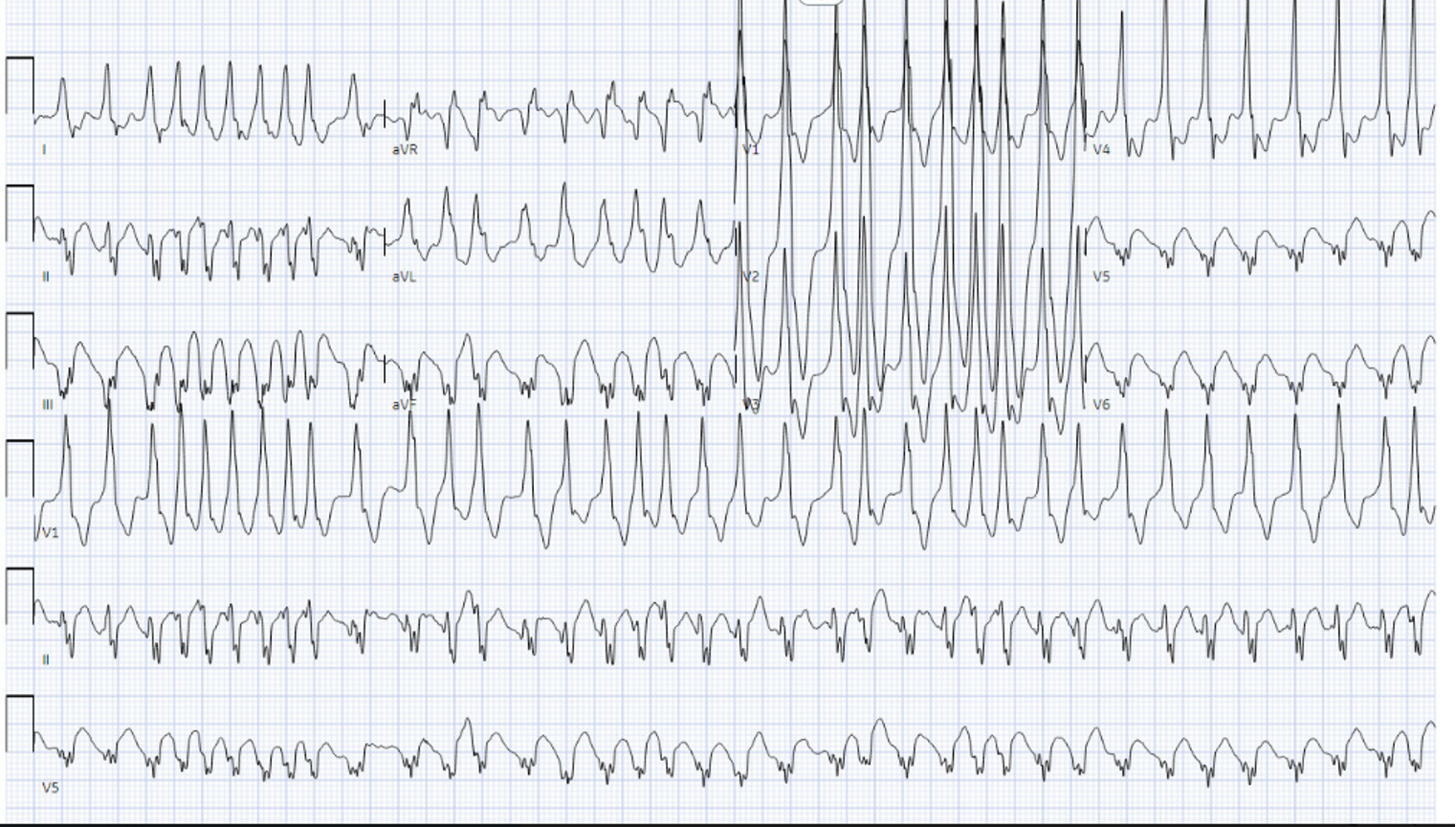
The ECG shows an irregularly irregular tachycardia with no organised p wave activity consistent with atrial fibrillation (AF). The QRS complexes are broad with a slurred upstroke/downstroke to the QRS complex (circled) as the ventricle is initially depolarised via the accessory pathway rather than the AV node and the His-Purkinje system.
An accessory pathway is an alternate electrical connection between the atria and the ventricle that does not utilise the AV node and the His Purkinje system. The AV node has the ability to decrement, i.e. it can slow or block conduction when it receives rapid electrical signals such as in AF, a key safety feature.
Many accessory pathways lack this property and therefore allow the conduction of rapid atrial signals to the ventricle that can cause ventricular fibrillation and sudden cardiac death.
This patient appears to have an accessory pathway that is capable of conducting at very rapid rates (note the very short RR interval ~4 small squares between complex 8 and 9- [star]) making it a malignant or dangerous pathway. This can be a potentially lethal arrhythmia.
Initial management consists of electrical cardioversion in the emergency department. AV nodal blocking agents, particularly adenosine should be avoided.
Following cardioversion, her sinus ECG demonstrated manifest preexcitation with short PR interval (<120ms), broad QRS with a delta wave.
The most definitive treatment option for this patient is a catheter ablation procedure to the accessory pathway. This should be performed as an inpatient given the potentially life-threatening arrhythmia observed. This procedure has a high chance of success (95%) and overall low risk of complication (3%). The procedure is focused at localising and abolishing the dangerous accessory pathway connection.
Atrial fibrillation is significantly more prevalent in patients with Wolf Parkinson White Syndrome (WPW) than the general population. It is thought that the presence of the accessory pathway is integral to the mechanism of AF pathogenesis in this population. In a young patient with clinical atrial fibrillation, WPW should be suspected. Similarly, unlike conventional atrial fibrillation patients, isolation of the pulmonary veins is not usually necessary in this cohort. After ablation of the accessory pathway, atrial fibrillation is not usually observed again.
Wrong answer! Please refresh page and try again