This content is part of a paid partnership with Medtronic.

 Aortic stenosis symptoms can often be overlooked as normal signs of ageing, but GPs should reach for their stethoscope to avoid underdiagnosis of Australia’s most common heart valve disease.
Aortic stenosis symptoms can often be overlooked as normal signs of ageing, but GPs should reach for their stethoscope to avoid underdiagnosis of Australia’s most common heart valve disease.
Early aortic stenosis often goes undiagnosed and without valve replacement prognosis can be abysmal, according to interventional and structural heart cardiologist Dr Gerald Yong.
Dr Yong is the head of the Valve Intervention Program at Fiona Stanley Hospital and operates privately at The Mount, Hollywood and Murdoch hospitals.
Much of his time in the theatre is spent completing transcatheter valve replacement and repair procedures that provide patients a chance of a healthier future.
So, what should GPs know about aortic stenosis?
Aortic stenosis is Australia’s most common heart valve disease. It affects one in eight patients over the age of 75, with age being one of the main risk factors.
Dr Yong said: “Essentially over 10% of elderly populations could have severe early stenosis or other serious heart valve disease.”
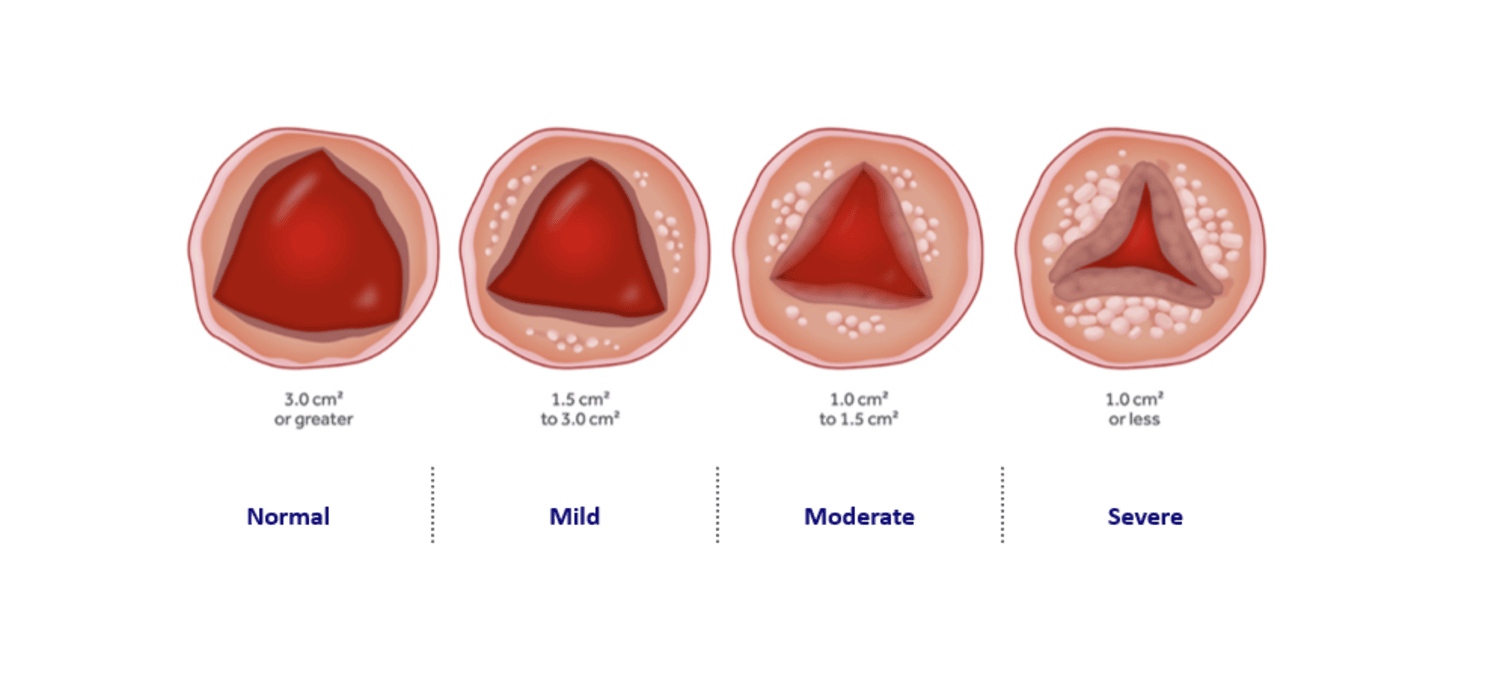
It occurs when the aortic valve hardens, reducing blood flow and placing strain on the heart. If left untreated, it can lead to heart failure.
And here is why it is not always picked up.
The main presentation is exertional symptoms such as exertional shortness of breath or chest pain, which are also typical symptoms that are associated with ageing.
Even before patients see their GPs, many will have spent time dismissing symptoms such as breathlessness, fatigue, or dizziness as normal ageing, which inevitably delays diagnosis and treatment.
Not only is aortic stenosis often put down to age, but it is sometimes mistaken for asthma.
Dr Yong said shortness of breath, chest discomfort, syncope, and reduced exercise tolerance should all prompt further investigation.
That’s why if he gets a chance to speak with GPs Dr Yong always reminds them of the importance of getting out a stethoscope.
“When you get these patients in, at least listen to their heart for a murmur,” he said.
“When you hear a murmur, investigate that by doing an echocardiogram. If you do that you are less likely to under diagnose the condition.”
Free heart checks
Are your patients over 65 and feeling short of breath, lightheaded or weary?
These could be the signs of a common underlying heart valve disease, such as aortic stenosis.
On Tuesday February 17 between 9am and 5pm, Hollywood Private Hospital will be hosting Free Heart Checks for patients over 65 experiencing these symptoms.
Bookings can be made via the Hearts for Hearts website or via Medtronic here.
Early intervention is key
As with most things in medicine, early referral to an interventional cardiologist was a key step to successful patient management.
“Early engagement with cardiology teams can significantly improve outcomes,” Dr Yong said.
“Once you’ve developed a severe aortic stenosis with symptoms, it is a clear-cut indication that you need valve replacement. Without it, your prognosis is abysmal.
“We’re talking about one to two years mortality at 50%, which is actually worse than cancer, and the only way to reverse that is a valve replacement.”
Dr Yong started the Transcatheter Aortic Valve Replacement (TAVR) program in Western Australia some 15 years ago.
“Prior to that, the only way to treat aortic stenosis was open heart surgery to replace the valve,” Dr Yong explained.
“More and more now we are doing transcatheter valve replacement.”
GPs can encourage patients to maintain heart health through:
- Blood pressure and cholesterol management
- Regular physical activity
- Smoking cessation
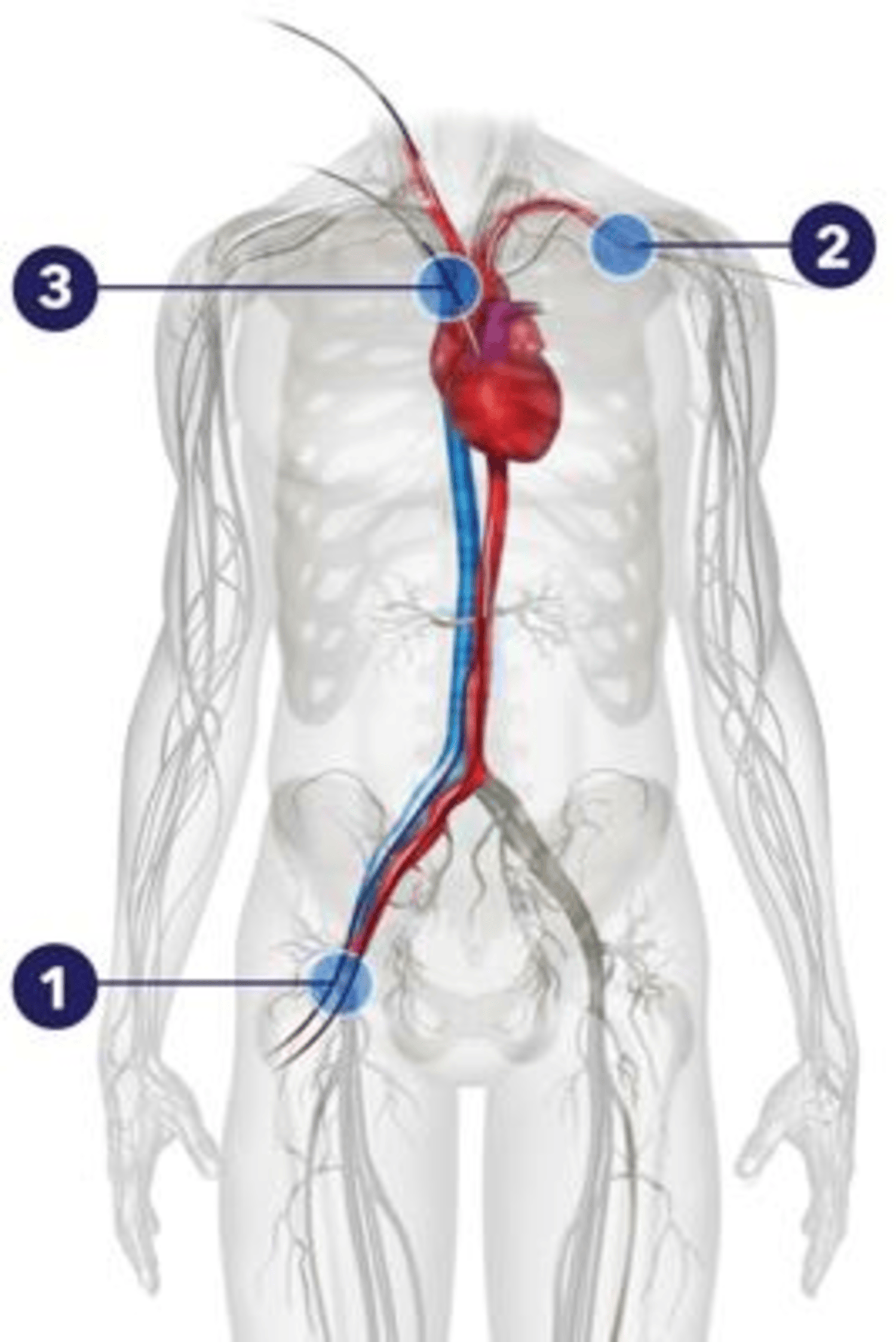
The procedure sees a new valve made of animal tissue guided into place through keyhole surgery and expanded, pushing the old valve aside.
“We can replace the valve through the TAVR procedure, where we essentially push the valve through a small puncture in the femoral artery all the way to inside the native aortic valve,” he said.
“We then expand the transcatheter valve and it pushes away the native valve.”
Dr Yong said this procedure offers far less trauma and recovery time than open heart surgery.
In fact, the majority of procedures are undertaken while the patient is awake under local anaesthesia, rather than general anaesthetic.
Ensuring patients are fit for procedure
Structural heart nurse Cecilia Wong is an integral member of Dr Yong’s multidisciplinary structural heart team, which provides comprehensive assessment and care for patients being considered for TAVR.
animal tissue guided into place through
keyhole surgery.
Patient evaluation is thorough and collaborative, commonly involving interventional cardiologists, cardiac surgeons, cardiac imaging specialists, and geriatricians. The assessment process includes advanced investigations such as CT imaging and coronary angiography, alongside functional and frailty assessments, to ensure patients are optimally selected and prepared for the procedure.
Care is delivered within a structured multidisciplinary framework, incorporating formal heart team discussions, coordinated peri-procedural management, and post-procedural rehabilitation supported by allied health professionals. Ongoing follow-up includes clinical review and echocardiographic surveillance to ensure optimal long-term outcomes.
The European Society of Cardiology has recently updated its guidelines to recommend TAVR for patients aged 70 years and older, expanding access to this minimally invasive treatment for a broader patient population.
Dr Yong’s private practice is iSave Heart Clinic, located at Suite 52, Wexford Medical Centre, 3 Barry Marshall Parade, Murdoch WA.
Want more news, clinicals, features and guest columns delivered straight to you? Subscribe for free to WA’s only independent magazine for medical practitioners.
Want to submit an article? Email editor@mforum.com.au