 Next-generation technology from SA has proved it can eradicate some of the most notorious and potentially deadly bacteria in the world.
Next-generation technology from SA has proved it can eradicate some of the most notorious and potentially deadly bacteria in the world.
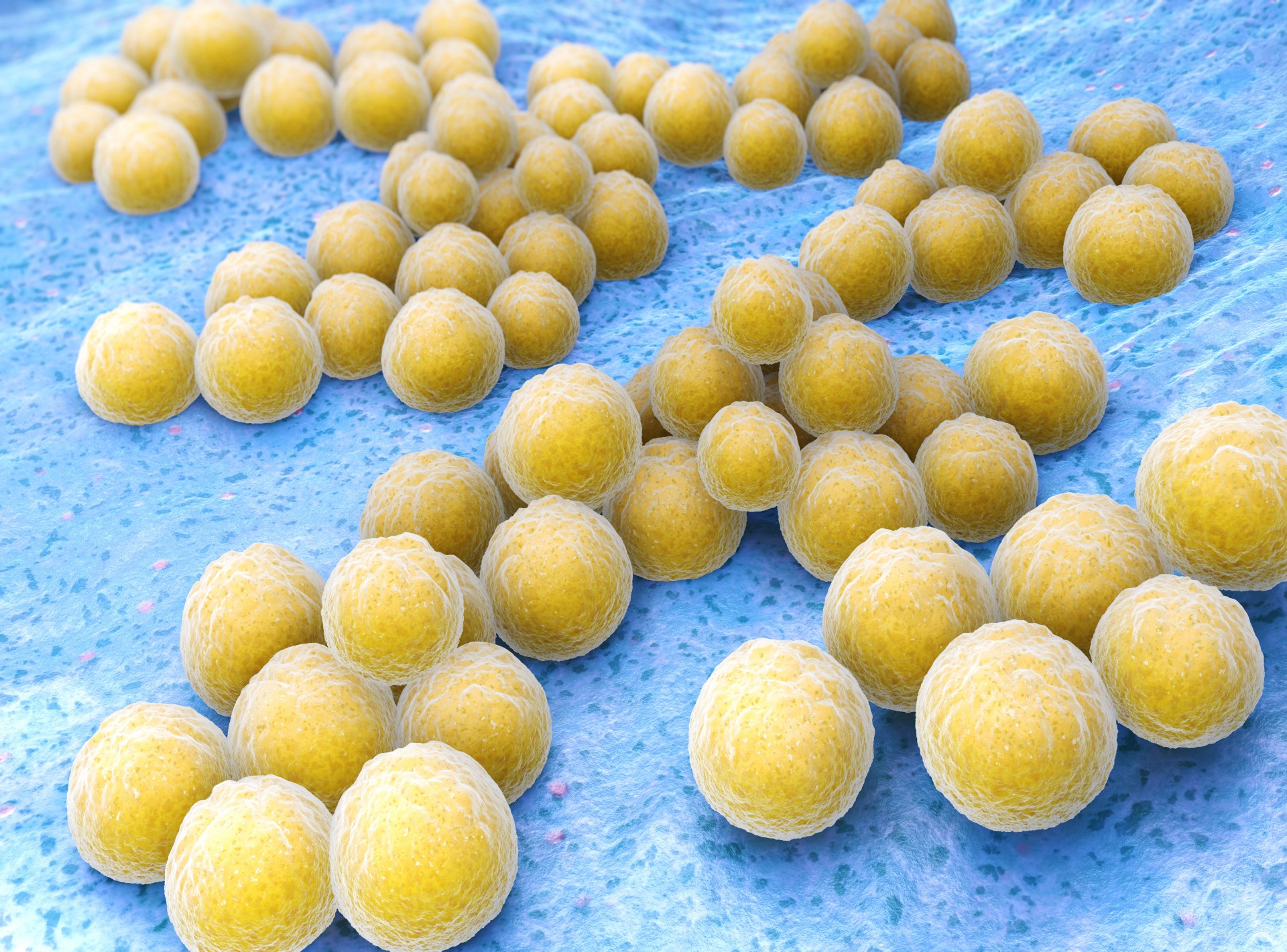
The study, published 6 October 2022 in Pharmaceutics, demonstrated that the new light-activated, nanotech therapy, developed by the University of South Australia, can eliminate antibiotic-resistant superbugs Staphylococcus aureus and Pseudomonas aeruginosa by 500,000-fold and 100,000-fold, respectively.
Lead researcher, University of SA’s Dr Muhammed Awad, explained that antimicrobial photodynamic therapy (aPDT) has evolved as a treatment paradigm to control the looming number of multi-drug resistant microbes and believed that their new light therapy will be a game-changer for millions of people worldwide.
“Patients in hospitals – particularly those with wounds or catheters, or those on ventilators – have a higher risk of getting these bacteria, and while antibiotics may help, their extensive use has led to waves of microbial resistance, often making them ineffective,” Dr Awad said.
“The new therapy is created in an oil that is painted on a wound as a lotion. When laser light is applied to the lotion, it creates reactive oxygen species which act as an alternative to conventional antibiotics.”
Pseudomonas aeruginosa is an opportunistic Gram-negative pathogen notorious for its biofilm formation and intrinsic resistance to multiple drugs, thanks to an outer lipopolysaccharide membrane that limits the penetration of xenobiotics to the cytoplasm and efflux pumps that expel antibiotics out of the bacterial cells.
When in biofilms, pseudomonas aeruginosa live as aggregated colonies embedded within extracellular polymeric substances (EPS), and the complex nature of EPS allows pseudomonas aeruginosa to escape host immune response and hinders antibiotics reaching the embedded cells.
“Our photodynamic technology works differently, harnessing the energy of light to generate highly reactive oxygen molecules that eradicate microbial cells and kill deadly bacteria, without harming human cells,” Dr Awad said.
“Unlike antibiotics, aPDT attacks multiple targets of microbial cells, limiting their ability to develop resistance. The concept of aPDT is to utilize reactive oxygen species (ROS) generated from the interaction between visible light and nontoxic dyes, termed photosensitisers, to inactivate target cells.”
The photosensitization process is akin to luminescence, where the electrons of photosensitisers transition from the ground state to excited states upon light illumination.
These electrons undergo intersystem crossing, where the released energy can be transferred to molecular oxygen, generating highly reactive singlet oxygen, or undergo chain reactions, generating other ROS, such as hydroxyl and superoxide radicals.
“These molecules target multiple bacterial cells at once, preventing bacteria from adapting and becoming resistant,” Dr Awad said.
“It is a far more effective and robust treatment, and importantly, the human skin cells involved in the wound healing process showed enhanced viability, while the antibiotic resistant bacteria were entirely eradicated.”
Co-author, Professor Clive Prestidge, explained that their third generation of photosensitisers was developed by loading existing photosensitisers into smart nanocarriers that enhanced their bioavailability and targeting of cancer and microbial cells.
“The main goal of utilizing nanoparticles in the field of aPDT is to improve the biological activity of hydrophobic photosynthesisers, such as gallium protoporphyrin (GaPP), by enhancing their solubility in biological media,” he said.
GaPP had been proposed as a photosensitiser against S. aureus, as its structural similarity with heme enables its superior uptake, compared to other porphyrins, through heme acquisition pathways, an uptake mechanism that potentiates its antibacterial activity as an iron mimetic agent in the dark and as photosensitiser upon light activation.
However, the versatile approaches to acquiring iron by different bacterial species and the hydrophobicity of GaPP lowered its potential as a photosensitiser for antimicrobial applications.
“Current photoactive compounds suffer from poor water-solubility which mean that they have limited clinical application, and our approach uses food grade lipids to construct nanocarriers for the photoactive compound which improves its solubility and antibacterial efficiency far beyond that of an unformulated compound,” the researchers said.
The SA team tested the optimization of GaPP using liquid crystalline lipid nanoparticles (LCNP) as a medium for the effective application of the photosensitiser against Pseudomonas aeruginosa, a more challenging biological target, assessing its broader application as photosensitiser in aPDT.
The LCNP was prepared using the hydrotropic dilution method: glycerol monooleate (15 mg) were mixed with Pluronic F127 in powder form (3 mg) and propylene glycol (0.26 g) via vortexing for 2 min in a 15 mL glass vial to form a homogenous gel, followed by the addition of 0.5 mL methanolic solution of GaPP (1.5 mM).
An amount of 3 mL methanol was added to ascertain the solubilization of the mixture, and a stream of nitrogen gas was used to obtain a dry film of GaPP/lipid before the dry film was dispersed in Milli-Q water to form a nanoparticle dispersion with a final volume of 5 ml.
Key parameters affecting the photodynamic activity of GaPP-LCNP against P. aeruginosa – light dose, GaPP concentration, and incubation time – were optimized to achieve maximum bacterial inactivation.
Maximum antibacterial activity was achieved at a light dose of 17.2 J.cm2, where the viability of P. aeruginosa culture was reduced by ~7 log10, and a total GaPP concentration of 0.8 M in the LCNP reduced the viability of P. aeruginosa by another ~7 log10.
“Moreover, the successful entrapment of GaPP within the LCNP bilayer modulated its optical properties, evidenced by higher absorption.” the researchers said.
“Further increase in GaPP concentration did not significantly improve the antibacterial activity, rather a decline singlet oxygen quantum yield from 0.72 to 0.33 was recorded at 15 M concentration, which can be ascribed to the photobleaching of GaPP by the generated oxygen.”
Finally, the GaPP-LCNP were incubated with P. aeruginosa in the dark for different periods of time before photoinactivation, with viability assessed using CFU enumeration, revealing that a total of 30 min pre-incubation time was necessary to reduce the viability of P. aeruginosa by ~7 log10, with shorter and longer incubation periods proving ineffective.
“These findings strengthen our claim of using GaPP-LCNP as a third-generation photosensitiser against Pseudomonas biofilms that offer remarkable antibacterial activity with a high safety profile,” the authors concluded.
“Several factors contribute to the higher antibacterial activity of GaPP-LCNP. Firstly, the liquid crystalline structure of the nanoparticles that protect GaPP from aggregating in biological media, maximizing GaPP light absorption and ROS production.
“Secondly, the attachment of LCNP to Pseudomonas biofilms forming a coating patch that helps overcome come reactive singlet oxygen’s limitations of short lifetime and short diffusion length (3.5 s and ~100 nm).
“Thirdly, despite their negative charge, LCNP can alter P. aeruginosa cell wall permeability via quick fusion with bacterial outer membranes, such as cationic entities. All these mechanisms combined qualifies GaPP-LCNP to be a promising photosensitiser against resistant localized infections.”
“This technology is very promising and is gaining the attention of scientists worldwide,” Prof Prestidge added.
“The next step is to commence clinical trials and develop this technology further to be available in clinics. With the support of funding bodies, we hope that Australians will have access to this technology as soon as possible.”

