Endocrine causes of secondary hypertension.
By Dr Jonathan Grasko, Consultant Chemical Pathologist & Toxicologist, Clinipath Pathology
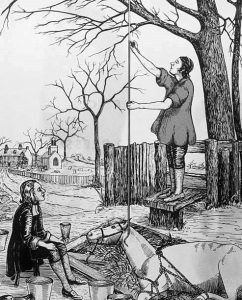
As far back as 2600 BC during the reign of the Yellow Emperor of China, the health of the heart, the essential vital organ could be assessed by using the pulse. A disease state of the heart called “hard pulse disease” was treated with venesection and bleeding by leeches. Sorovas of Ephesus in 120 AD felt that “hard pulse disease” was due to animal spirits and the only cure was to draw them down and out by cupping of the spine. However, it was not until Stephen Hales’ discovery of blood pressure in 1733 and the subsequent description of the pathology of the disease by Thomas Young in 1808 that hypertension entered the clinician’s psyche.
As early as 1900 the insurance industry provided consistent evidence of the risk of high blood pressure. In 1911, the medical director of the Northwestern Mutual Life Insurance Company wrote, “The sphygmomanometer is indispensable in life insurance examinations…”
Serial publications by the Actuarial Society of America meant there was no doubt that mortality for both men and women rose with an increase in blood pressure.
Despite extensive research, the aetiology of hypertension for most patients has remained elusive (with only about 5-10% having a definable aetiology as secondary hypertension – including drugs and renal/renovascular diseases and less than 1% of hypertensive patients due to endocrine dysregulation.)
Endocrine induced hypertension is of exceptional importance as it is the only group which is amenable to definitive treatment with the promise of cure and therefore should always be excluded.
Here, I outline biochemical investigation of secondary causes of hypertension due to endocrine dysregulation.

Hyperthyroidism
Due to excessive circulating thyroid hormone; common signs and symptoms may include irritability, muscle weakness, sleeping problems, a palpitations/tachycardia, hypertension, heat intolerance, diarrhoea, enlargement of the thyroid and weight loss.
Screening and Confirmatory Investigations:
- Thyroid function tests (TSH, Free T4 and Free T3)
- Thyroid antibodies (TPO and TSH receptor antibodies)
Primary aldosteronism (Conn’s syndrome)
Autonomous production of the aldosterone by the adrenal glands which results in excessive sodium and water retention and therefore hypertension.
Screening Investigations:
- Serum Aldosterone: Plasma Renin ratio
- result affected by antihypertensive drugs
- false positives with B-blockers
- false negatives with angiotensin converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARB’s) and if hypokalaemic, confirm normokalaemia prior to testing
- result affected by antihypertensive drugs
Confirmatory Investigations:
- Saline suppression of aldosterone test
- Adrenal vein sampling to lateralise aldosterone production.
Hypercortisolism (Cushing’s syndrome)
Extended exposure to excessive glucocorticoids, which may result in in some of the classic features that include high blood pressure, central obesity, red/purple striae, moon facies, buffalo hump, muscle weakness, osteoporosis, easy bruising and poor wound healing.
Screening Investigations:
- 24 hr urinary free cortisol ( preferred for patients on the oral contraceptive pill and certain antiepileptic drug)
- Low dose dexamethasone suppression test (preferred screening test for adrenal adenoma)
- Late night salivary cortisol (2 measurements)
Confirmatory Investigations:
- Low dose/High dose dexamethasone suppression test
- Petrosal sinus sampling
<subhead>Phaeochromocytoma
Pheochromocytoma and paragangliomas are neuroendocrine tumours most commonly located in the medulla of the adrenal glands. They result in uncontrolled and variable release of catecholamines (adrenaline and noradrenaline), which makes clinical diagnosis difficult. Classical features, which are not always present include tachycardia, palpitations, hypertension, diaphoresis (excessive sweating) and headaches.
Screening Investigations:
- Plasma free metanephrines
- Urine fractionated metanephrines
Confirmatory Investigations:
- Clonidine suppression test
Acromegaly
Excess growth hormone is secreted by the pituitary gland after the growth plates have closed. The initial symptoms are typically enlargement of the hands and feet, followed by enlargement of the forehead, jaw and nose. Long term sequelae may include Type 2 Diabetes, sleep apnoea, and hypertension.
Screening Investigations:
- Insulin-like growth factor 1 (IGF-1)
Confirmatory Investigations:
- Glucose suppression of growth hormone.
Hypertension, the most insidious and surreptitious of diseases, may with the insight cleaved from endocrine induced hypertension, finally extinguish this scourge that is “hard pulse disease”.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

