Love them or hate them, tattoos might be a doctor’s best friend. Scientists in Germany have reportedly developed three tattoo dyes that change colour based on the levels of certain health markers in the blood. One of the dyes responds to pH, and gradually changes between yellow and blue depending on whether the blood is more or less acidic. In a healthy scenario, the pH-measuring tattoo ink would always look dark green. Another dye reacts to changing glucose levels by changing from light green to dark green and could help people manage their diabetes. The third dye moves between shades of light blue based on the level of albumin in the blood, which is of particular interest to people who are at risk of liver failure or kidney failure. Don’t prescribe tatts to your patients just yet. The researchers are yet to determine if the colour changes are reversible. So far only the pH marker turns back to its original colour. And questions hang over people with different skin tones, how safe are the dyes and are they colourfast. The small stuff!
AMA plays a trump
Negotiations around the seventh Community Pharmacy Agreement (CPA) have produced some dazzling moves by various groups, the best must be attributed to the AMA federal council. In a hard, low and flat backhand at the feet of the Pharmacy Guild, the council resolved to develop a blueprint on drug dispensing models that could see GP ownership of pharmacies and dispensing medications from general practice. The statement said this would offer patients “enhanced convenience, safety, and quality care in their access to medications”
The national president GP Dr Tony Bartone said “Incorporating pharmacy services into general practice, under the ownership of a medical practitioner, would improve patient care by allowing GPs to lead a team of co-located health professionals in providing multidisciplinary health care to patients at the local community level,” he said. “Many general practices already provide co-located services with pathology collection centres, and in-house psychologists, physiotherapists, dieticians, and podiatrists. Adding pharmacy to the mix would have benefits for patients, pharmacists, and GPs.”
Both federal and state governments have announced their support for a broader scope of practice for community pharmacies, hence the greenlight for them to deliver a range of vaccinations beyond the flu vax and even patient consults in some areas. This, understandably, hasn’t gone down well with GPs.
Rhetoric from the doctor groups has moved beyond the initial salvos of “if pharmacist want to practise medicine, they should get a medical degree” and “pharmacists should stick to their perfumes and probiotics” to harder ball.
The Pharmacy Guild has been described in some media reports as one of the most powerful lobby groups in Australia. The former ACCC chair Prof Graeme Samuel is reported as saying the guild had engaged in “straight political blackmail” and “unashamed” lobbying in the past to maintain an anti-competitive regime.” Docs will need to be on their mettle.
The 18-month state-based GP Urgent Care pilot kicked off in September with 125 practices participating, which Health Minister Roger Cook says will give 70 postcodes access to urgent care with a local GP. In June, we reported the GP pushback to St John Ambulance’s federally funded urgent care centres. While there has been no announcement by either the federal government or St John Ambulance as to whether they were successful in securing the election commitment of $28 million, it hasn’t deterred the State Government, in collaboration with WAPHA (and the support of the RACGP and the AMA), to set the course for this more modestly priced pilot using the resources of private general practices. We’ve heard that Brecken Health will lead the charge in the Bunbury region, so the pilot is also hitting the regions. It is, of course, the state government’s desire to take pressure off emergency departments by having urgent care (simple fractures and wound care) delivered in the community. The program will be evaluated by UWA and Curtin academics. The government says that in 2017-18, 190,000 attendances to hospital EDs could have been treated by GPs. Participating GP practices in the state pilot will have access to pathology and radiology services and have fully equipped treatment rooms. GP Urgent Care appointments can be accessed between 8am to 8pm, seven days a week. These hours were determined by using records of ED presentations for these non-life-threatening conditions – most of which occur during the day. A sample of the day in the life of an Urgent Care GP could be seeing patients with gastrointestinal illnesses, musculoskeletal and orthopaedic injuries, ENT conditions, stings, rashes and wound infections and abrasions and minor lacerations. Appointments can be made online at http://gpurgentcare.com.au or by calling HealthDirect on 1800 022 222.
Killer asbestos
Last month we began our exploration of the re-emergence of silicosis as an industrial hazard and we continue this month with an interview with a stonemason who contracted the disease over his 33-year career. Links are also being made to the ban asbestos campaign when mesothelioma raised its ugly head. Australians continue to bear the burden of asbestos-related disease. The AIHW released its latest report which showed that 699 people died in 2018 from mesothelioma. There were also 662 new diagnoses last year in people aged between 22 and 101 years. This is despite asbestos, in all its forms, being banned in Australia since 2004. “The ‘average’ Australian with mesothelioma was male, diagnosed at around 75 years of age, exposed to asbestos in occupational and non-occupational settings and lived for around 11 months after diagnosis,” the report said. WA had the highest standardised rate between 2015 and 2018 with 4.4 cases per 100,000 people.
Black hole of self-reporting
In the September issue we spoke to immunologist and allergist Dr Michaela Lucas. Her particular interest is around drug allergies, especially antibiotics. At the recent conference of the Australasian Society of Clinical Immunology and Allergy (ASCIA) in Perth, Dr Lucas reported that 90% of people who self-reported an allergy avoided taking certain antibiotics, which restricted prescription choices for doctors when treating infections and led to the emergence of super bugs. While the process of reporting and creating an antibiotic allergy label was important to protect patients from serious adverse reactions, if the reported reaction was not further investigated and confirmed, the label could be incorrect. “It is estimated less than 10% of adult and paediatric patients carrying an ‘antibiotic allergy’ label are truly at risk of a significant allergic or adverse reaction,” Dr Lucas said. “We also urgently need to increase resources to enable patients to seek specialist advice to allow for a medical assessment of their drug allergy status.”
The WA Kirkbride Melanoma Advisory Service (WAKMAS, formerly WAMAS), is holding its second annual GP education evening at the Harry Perkins Institute for Medical Research in November. The service’s director Dr Mark Hanikeri will give an overview of the service before a program of topics from WAKMAS referral pathways to clinical topics such as advances in treatment of stage 3 melanoma, surgical management and future developments for diagnosis and treatment. There will be plenty of time for questions. The evening will be held on Tuesday, November 12, 2019, commencing at 7pm concluding around 9pm. Entry is free. This sponsored event is usually over-subscribed and seats are limited so please save the date and confirm attendance early.
The fat gene switch
The WA Raine Study treasure trove is the backbone of a UK/Finland study which has found that the body mass index (BMI) in babies, children and adults is influenced by different genetic factors that change as we age. Researchers found that BMI in babies was influenced by a distinct set of genetic variations that played little role in determining weight in later life. However, some genetic variants associated with adult BMI started playing a role during childhood from around the age of four to seven years old, suggesting that the origins of obesity in adults might lie in this critical stage of childhood. Senior author Prof Marjo-Riitta Jarvelin, from Imperial College London, said the study showed that nearly 100 genetic variations, which increased a person’s risk of obesity in adulthood, seemed to start taking effect from around the age of four. “Environmental factors like the food we eat and our lifestyle have an increasing impact on obesity development as we age,” she said. “These external factors seem to unmask, gradually, the genetic contributors to obesity that we have from early life, programming development towards an unhealthy direction.”
Needing clear air
Former Curtin University professor Dr Linda Selvey, who is president of the Australasian Faculty of Public Health within the Royal Australasian College of Physicians, has joined the chorus urging the government to revise air pollution limits. She says air pollution contributes to asthma, heart disease, lung disease and cancer. “Australia’s air pollution limits haven’t changed in 21 years. Our current air pollution restrictions far exceed the recommendations set by the World Health Organisation, so we must take urgent action to protect our community,” she said. She pointed to data that suggested over 3000 premature deaths a year are caused by ambient air pollution in Australia. Nitrogen dioxide and sulphur dioxide are largely released from vehicle emissions and coal-fired power generation respectively.
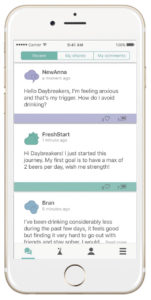
The National Drug Research Institute (NDRI) based at Curtin University has just published an evaluation of the Daybreak digital app, which has been developed as an intervention to support high-risk drinking individuals looking to change their relationship with alcohol. The study, which was published in the Journal of Medical Internet Research, found that with three months consistent use it helped both “risky/harmful” and “probably dependent” drinkers – the most complex cases to treat.
The evaluation involved 793 Australian adults and found that the 70% of participants classed as “probably dependent” more than halved their alcohol consumption while using Daybreak, from 40.8 standard drinks a week to 20.1 standard drinks. Alcohol consumption among “risky/harmful” drinkers dropped from 22.9 standard drinks a week to 11.9 standard drinks, which is below NHMRC guidelines that recommend no more than 14 drinks a week.
NDRI’s Dr Robert Tait said that those who stayed engaged with the Daybreak program showed remarkable reductions in their alcohol consumption.
“While our evaluation only focused on a small group of people over three months, the reductions in alcohol consumption achieved indicate the potential for online interventions to help people with more entrenched alcohol problems, which is particularly significant given the wide potential reach of online interventions.”
Since 2016, Daybreak has been available across the PHN network, and since 2018 it has been funded by the Federal Government with an initial $3m investment. More than 5000 app users remain active in the program each month.
https://www.ncbi.nlm.nih.gov/pubmed/31486406
Cancer perceptions
What role does fate play when it comes to the perceptions of 145,000 people diagnosed with cancer each year in Australia? Quite a lot it seems. Despite the multitude of warnings on the cancer-related dangers of smoking, sun exposure, poor diet, alcohol consumption and inadequate exercise, it seems, going by research by the University of Newcastle and Vietnam Cancer Institute, the message isn’t getting through. A study of Australian cancer patients identified ‘bad luck’ or fate as the third most commonly perceived cause of their cancer, behind age and family history. It compared the perceptions between 585 cancer patients in Australia and Vietnam, analysing differences across 25 possible beliefs about what may have caused their cancer. Almost half of the Australian cancer patients believed “getting older” was the main cause of their cancer, while most Vietnamese patients cited “poor diet” as the main contributing factor for their cancer. Overall, smoking was ranked fifth most likely cause and alcohol the ninth most likely cause.
ACCC hip and shoulder
To add to the complex concoction that is Australian private health insurance, the ACCC is chasing down Medibank Private in the Federal Court for alleged false representations about benefits covered by its health insurance policies. And not for minor procedures but for joint replacement. The ACCC alleges that Medibank falsely represented to over 800 members holding AHM “lite” or “boost” policies, who were making claims or enquiries, that they were not entitled to cover for joint investigations or reconstruction procedures, when in fact they were. “As part of our case, we estimate about 60 members needlessly upgraded their policies so they could access the joint investigation and reconstruction procedures they were already entitled to under their existing, cheaper insurance policies,” the Commissioner Rod Sims said. “In some cases, it is alleged that members who upgraded their policies were also required to serve a further waiting period to access these procedures,” Mr Sims said. He said the alleged misrepresentations had serious consequences for those members requiring procedures including spinal surgery, pelvic surgery, hip surgery and knee reconstructions. “Some members were forced to delay surgery due to high out-of-pocket costs…and to seek alternative remedies to manage pain, when they were in fact entitled to insurance cover,” he said. Medibank self-reported this conduct to the ACCC and has begun compensating affected members.
Women stand up
A new AIHW report that looks at the prevalence of and hospitalisations associated with endometriosis reveals that almost 7% of women aged 25-29 and 11% of women aged 40-44 have the condition. Researchers at the University of Queensland used data from the Australian Longitudinal Study on Women’s Health, along with health service data, to estimate the prevalence of endometriosis in two groups of women — those born in 1973-78 (with data available up until age 40–44) and those born in 1989-95 (data available up until age 25-29). Around one in 15 (6.6%) women born in 1989-95 were diagnosed with endometriosis by age 25-29 — a figure that is 1.7 times as high as that of women born in 1973-78 at the same age (4%). This increase may reflect increased awareness of endometriosis among women and doctors, leading to increased diagnosis and/or reporting of diagnosis among women born more recently. In 2016-17, there were about 34,000 endometriosis-related hospitalisations, 95% of which involved at least one procedure. The most common procedures included diagnostic hysteroscopy, and dilation and curettage. Endometriosis-related hospitalisations were more likely to be partly or fully funded by private health insurance than all hospitalisations for females (57% compared with 43%), and around twice as likely to be self-funded as all hospitalisations for females (7.9% compared with 3.6%).