 Middle-aged men over 45 will commonly be diagnosed as being overweight/obese, mildly hypertensive and having high cholesterol and/or triglycerides and impaired fasting glucose on blood tests. The doctor would then prescribe an antihypertensive medication and a statin and advise the patient that he needs to lose weight.
Middle-aged men over 45 will commonly be diagnosed as being overweight/obese, mildly hypertensive and having high cholesterol and/or triglycerides and impaired fasting glucose on blood tests. The doctor would then prescribe an antihypertensive medication and a statin and advise the patient that he needs to lose weight.

Managing metabolic syndrome by medical weight loss is an alternative option to commencing medication immediately on diagnosis.
The increasing prevalence of obesity has resulted in increasing prevalence of metabolic syndrome (MetS) affecting up to 25% of the world’s population and one in three people over 25 years in Australia.
MetS is a cluster of cardiovascular risk factors comprising central abdominal obesity, insulin resistance and dyslipidaemia associated with a proinflammatory and prothrombotic state. The clinical significance of MetS is that individuals with it are up to three times more likely to develop cardiovascular disease and up to five times more likely to develop Type 2 diabetes, than individuals without it
MetS is infrequently diagnosed in Australian general practice, possibly due to the fact that waist circumference is infrequently recorded (under 1 in 5 patients).
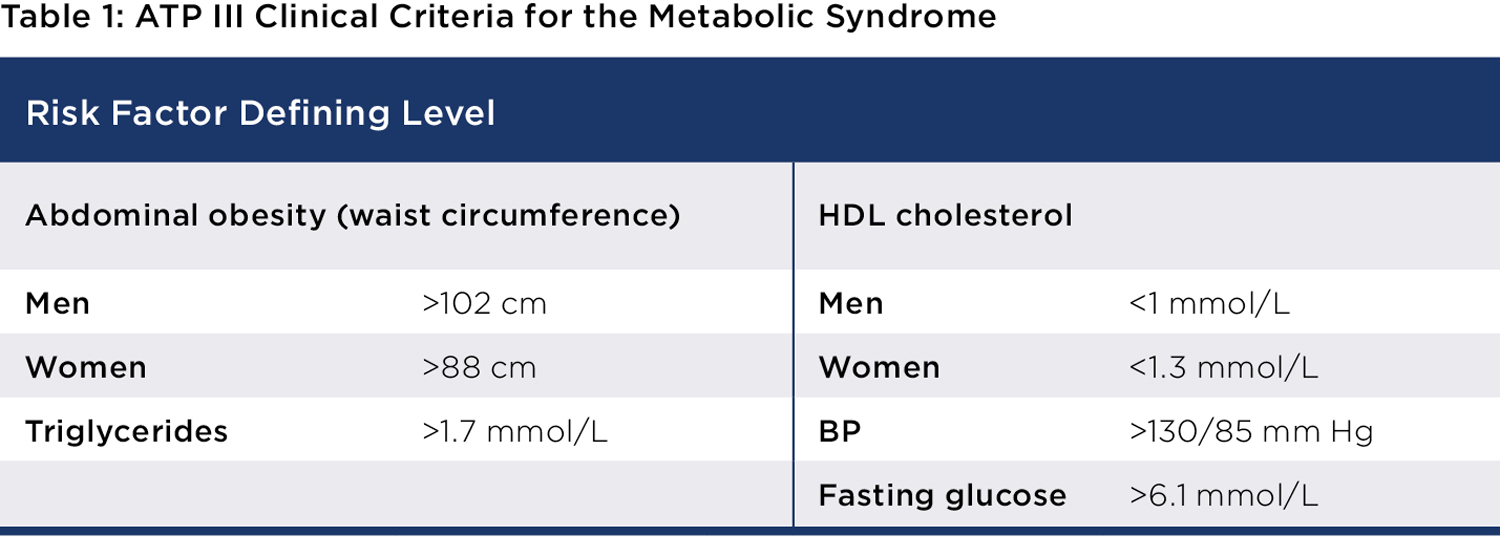
Abdominal obesity is more highly correlated with metabolic risk factors than elevated BMI. Therefore, measurement of waist circumference (WC) is important to identify abdominal obesity which is above 102cm (men) and above 88cm (women) (see Table 1).
The ideal management of MetS is weight loss and lifestyle interventions to reduce central obesity. The goal is to achieve a 5-10% or greater reduction in weight over 6-12 months. This can significantly reduce the severity of hypertension or dyslipidaemia, reduce cardiovascular risk and progression to Type 2 diabetes and reduce obesity-related co-morbidities. In more practical terms, weight loss may obviate the need for prescription of antihypertensive and statin medications.
Management approach
I find patients are often well motivated to commit to losing weight once they have been diagnosed with MetS, particularly when they realise that if they lose weight, they may not have to take antihypertensive or statin medication.
It is important to take a comprehensive weight history including factors which have led to weight gain (unhealthy eating habits, stress/comfort eating) and previous weight loss attempts.
Mental health problems such as depression and anxiety, sleep problems and stress management need to be addressed as these are major contributing factors to weight gain. There is a high incidence of obesity in patients
with mental health problems.
Review of the patient’s current medications is important to identify those that lead to weight gain. Common culprits in the antidepressant category are mirtazapine and sertraline, and antipsychotic medications such as olanzapine, clozapine, and quetiapine. Weight-neutral alternatives include escitalopram, desvenlafaxine and other SSRI/SNRI antidepressants and atypical antipsychotics (e.g., aripiprazole, lurasidone).
It is also important to address sleep problems and stress management, given that stress or comfort eating is a major source of weight gain for some patients.
Appetite suppressant medications can be considered to assist with weight loss. The choice of medication should be individualised to the patient.
 Weight loss medications
Weight loss medications
Phentermine is an adrenergic agonist which has side effects include insomnia, palpitations, and irritability. It is best avoided in those with anxiety and insomnia.
Bupropion/Naltrexone is a dopamine/noradrenaline reuptake inhibitor and an opioid receptor antagonist. It is a good choice for patients who are stress/comfort eaters and who drink a lot of alcohol, and who have some anxiety/depression as it reduces food and alcohol cravings, and bupropion is also an atypical antidepressant.
Liraglutide is a glucagon-like peptide receptor (GLP-1) agonist acting centrally to reduce appetite and increase satiety. Side effects include nausea, diarrhoea, constipation, and abdominal discomfort. It is a good choice for those who have a large appetite.
Topiramate and semaglutide are used off label. Combinations of medications (e.g., phentermine/topiramate.) can also be used.
Counselling about diet, exercise and behaviour change is critical. The aim is to reduce kilojoules by approximately 2100 a day whilst maintaining daily protein intake of approximately 1g/kg body weight, to reduce the risk of loss of muscle mass.
A very low carbohydrate diet (VLCD) using meal replacement shakes can be used for 12 weeks for rapid initial weight loss.
In summary, medical weight loss intervention resulting in loss of 5-10% or more of the patient’s initial weight has been shown to be effective in regressing hypertension, dyslipidaemia and insulin resistance associated with metabolic syndrome.
Key messages
- Metabolic syndrome is common but under-recognised
- Take a detailed weight history
- Medical weight loss is effective management.
Author competing interests- nil

