Breast cancer management has changed dramatically over the years. With overall survival rates now above 90%, safe de-escalation of surgery is now being emphasised, to minimise surgical morbidity and preserve aesthetic outcomes and quality of life.

Breast-conserving therapy (BCT) is breast-conserving surgery (BCS) and whole-breast radiotherapy. BCS can be performed with a simple, wide local excision for small cancers. Impalpable cancers can be identified surgically using a metallic clip marked with a guide wire prior to surgery, or increasingly a radioactive seed.
For larger cancers, oncoplastic breast surgical techniques allow for larger resections in smaller breasts, decreasing the need for a mastectomy. Oncoplastic BCS combines the oncological surgical principles with aesthetic plastic surgical techniques, improving cosmetic outcome without compromising local control.
Volume displacement oncoplastic BCS techniques rely on breast rearrangements to reshape the breast into a smaller size, after excising the cancer. A contralateral procedure may improve breast symmetry (e.g. therapeutic reduction mammoplasty is useful for large tumours in women with large pendulous breasts).
Volume replacement oncoplastic BCS techniques use local tissue to fill a breast defect when there is insufficient volume for displacement techniques, or when the patient does not want smaller breasts. Local perforator flaps are the most useful replacement techniques, consisting of excess subcutaneous fatty tissue adjacent to the breast laterally or inferiorly, which can be rotated into the breast defect as a flap on a pedicle supplied by an intercostal artery perforator.
Regardless of the BCS technique, tumour-free surgical margins (minimum 1mm for invasive disease, 2mm for DCIS) are essential. Involved surgical margins requires re-excision, with potential for delayed adjuvant therapy and increased patient anxiety. Very low (<10%) re-excision rates can be achieved in oncoplastic BCS with experienced teams in large volume breast cancer centres.

Final pathology: pCR breast (no invasive cancer) and axilla (19 benign lymph nodes) – current protocol would have recommended a targeted axillary dissection thus avoiding an axillary clearance.

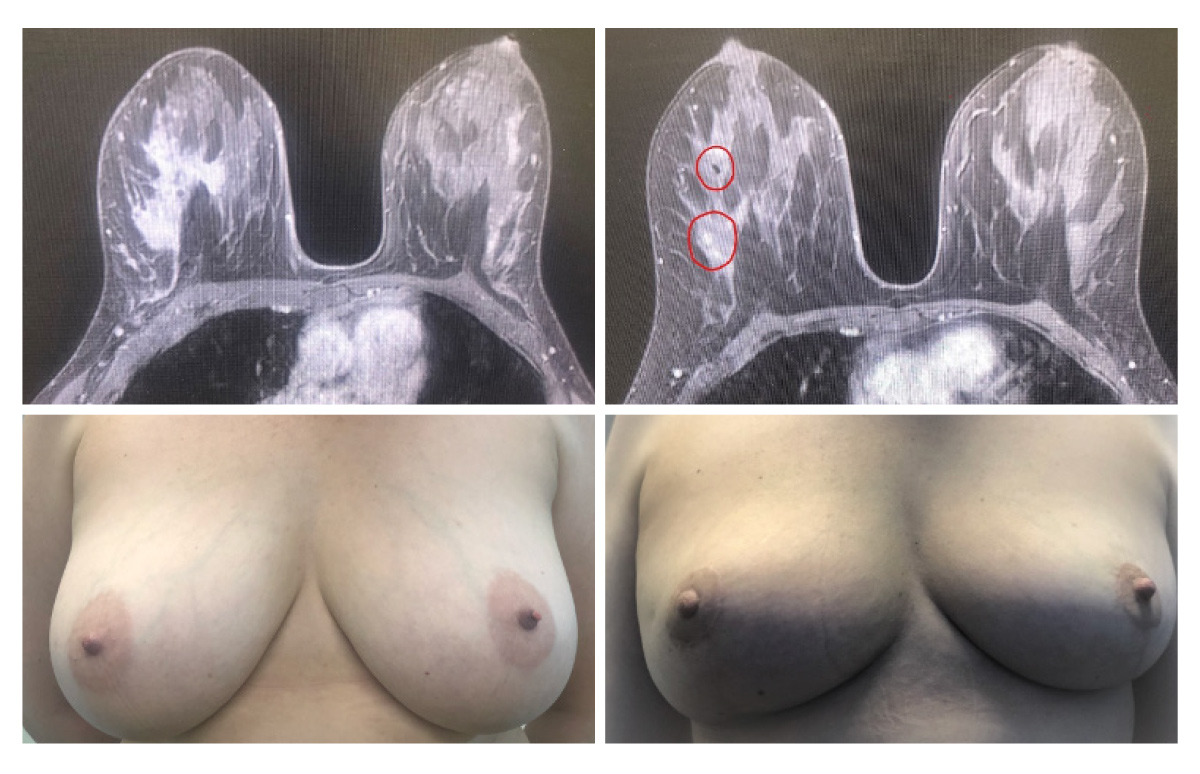
Preop (bottom left) and 5 months postop after bilateral reduction mammoplasties (bottom right – 350 gr of breast tissue removed right; 400 gr left) and right targeted axillary dissection, with postop right breast radiotherapy. Final pathology: pCR breast (no invasive cancer), residual high-grade DCIS with clear margins, 6 benign axillary nodes (2 with chemotherapy induced regression changes).
Neoadjuvant Chemotherapy (NACT), traditionally used for locally advanced or inoperable breast cancer, has been extended to downstage large tumours allowing BCS rather than mastectomy.
Tumour response to NACT is dependent on the histological subtype based on grade, ER, PR, and HER2 status. HER2-enriched cancers and triple-negative cancers have the greatest pathological complete response (pCR) rates. NACT is the preferred approach for these tumour subtypes, making them potential candidates for BCS, and more importantly, enabling additional chemotherapy for those with residual disease after completion of NACT and surgery.
When BCT is not possible, thoughtful planning of mastectomy, with consideration to breast reconstruction, is important for the emotional recovery from the trauma of breast loss. A skin-sparing, skin-reducing, or nipple-sparing mastectomy, with immediate reconstruction is a good option for selected women.
Reconstruction can be performed with implants as a one-stage direct-to-implant technique, or two-stage procedure with a tissue expander later changed to a permanent prosthesis. Implants can be placed in a pre-pectoral or sub-pectoral position.
Autologous tissue reconstruction involves pedicled or free-tissue transfer to the breasts. The deep inferior epigastric artery perforator (DIEP) flap uses tissue from the lower abdomen and is optimal in selected patients, although a more technically demanding procedure.
The trend to increasing rates of contralateral prophylactic mastectomy at the time of diagnosis of unilateral cancer is concerning, as this is associated with increased complications, and potential delays in cancer treatment, with no survival benefit.
In clinically node negative patients, the role of sentinel lymph node biopsy (SLNB) is a well-accepted, reliable method to assess the axilla, with limited arm morbidity compared to axillary lymph node dissection (ALND). A completion ALND can be safely omitted in patients with micrometastasis in the sentinel node(s), (i.e. 2mm or less). The extent of additional axillary surgery for those with a higher disease burden is a subject of ongoing discussion.
In clinically node-positive patients with HER2-enriched or triple-negative tumours, NACT allows for de-escalation of surgical treatment of the axilla. A targeted axillary dissection technique, consisting of a SLNB and specifically removing the affected nodes previously marked with a clip, can accurately restage the axilla after completion of NACT and identify the approximately 40% of women with nodal pCR who avoid a completion ALND.
Key messages
- Oncoplastic breast surgery allows more women to have breast-conserving surgery, wider resections, and less frequent involved margins
- Reconstruction options after mastectomy require careful planning and play a significant role in the psychological recovery from breast cancer
- Neoadjuvant chemotherapy downstages tumours to permit de-escalation of surgery in the breast and axilla.
Questions? Contact the editor.
Author competing interests: Nil.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

