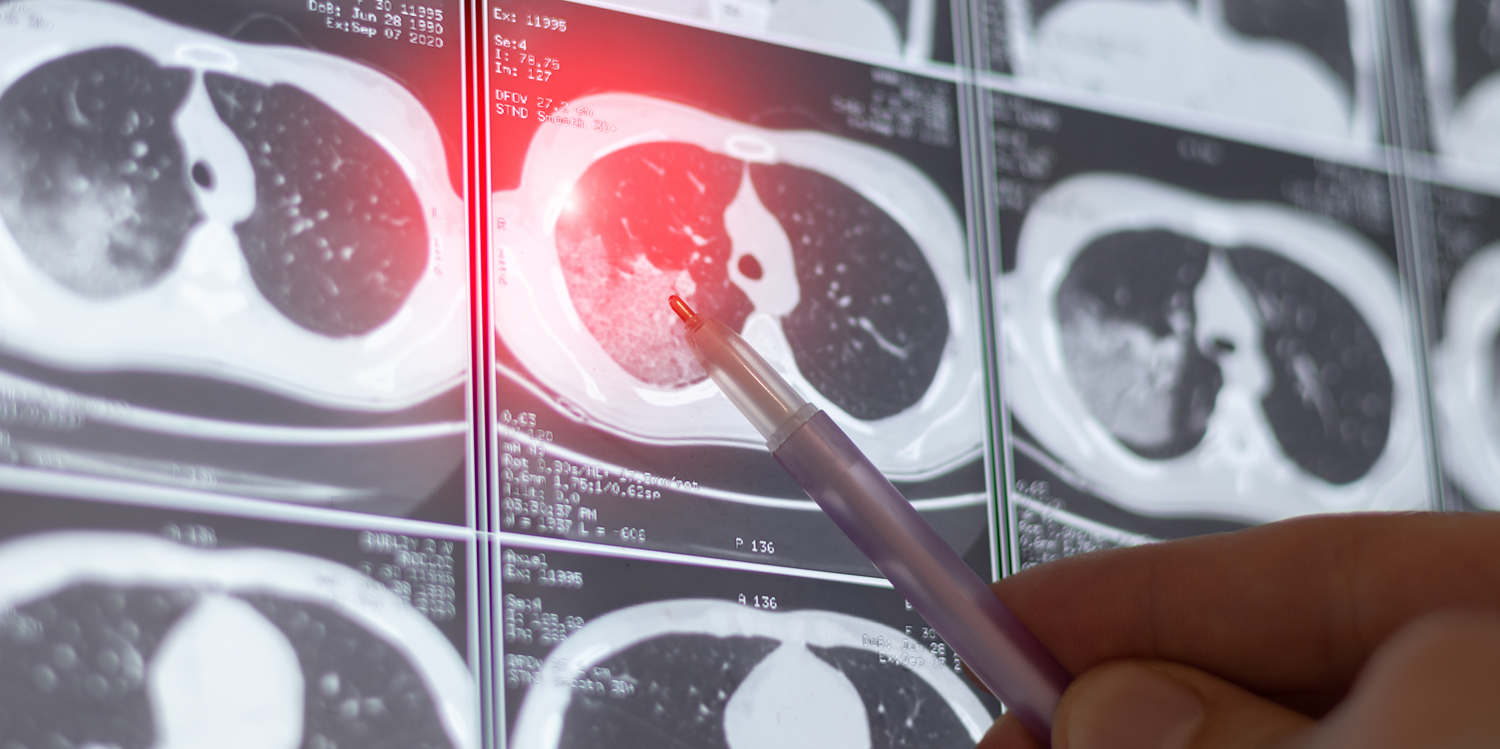
Patients battling lung cancer are expected to benefit from an Australian-first best practice guide to delivering optimal personalised treatment.
The Lung Cancer Molecular Testing Best Practice Recommendations aim to give patients access to the most appropriate molecular testing.
It is hoped that the new recommendations will avoid unnecessary biopsies, reduce treatment delays, and improve survival outcomes as well as help patients to live longer and healthier lives with fewer side effects.
Lung cancer is the fifth most commonly diagnosed cancer in Australia according to the Australian Institute of Health and Welfare. More than 1000 cases are diagnosed in WA annually.
When a person is diagnosed with lung cancer, special molecular or biomarker testing by pathologists helps determine the most effective treatment pathway.
The new best practice guide, developed by the Royal College of Pathologists of Australasia in collaboration with the Thoracic Oncology Group of Australasia, provides 16 recommendations on:
- Which molecular tests should be performed based on the type and stage of lung cancer
- When to conduct molecular tests to ensure timely treatment and the possible outcomes
- How to perform molecular tests to maintain high-quality, reliable results.
Lead author of the guide Professor Wendy Cooper said treatment had advanced significantly in recent years, resulting in increasingly complex treatment plans.
“Yet evidence shows that biomarker-driven therapies can significantly improve survival rates and treatment responses compared to traditional methods,” Professor Cooper said.
“Early and accurate identification of genetic mutations in biomarkers such as EGFR, ALK, ROS1, MET, RET, NTRK, HER2, BRAF, KRAS and PD-L1 enables patients to receive the most effective care with tailored solutions that are targeted specifically to their tumour, potentially avoiding less effective and toxic treatments.”
The new recommendations have been released ahead of the National Lung Cancer Screening Program, which will come into effect in July.
RELATED: Lung Cancer Screening program a game-changer for diagnosis
Lung Foundation Australia has expressed concern that stigma surrounding the disease may affect participation in the screening program.
It’s recent lived experience survey that found 57% of people living with lung cancer had experienced stigma.
Fifty-eight percent of respondents experienced distress because of stigma from healthcare professionals, with 26% indicating it was a barrier to healthcare.
The findings also showed an increased level of stigma since 2020, particularly from patients’ family, friends, and healthcare professionals.
Media content analysis by Daffodil Centre postdoctoral research fellow Dr Shiho Rose and her team found that stigmatising language such as blame-focused terms and moralising narratives remained prevalent in media coverage.
LISTEN: Lung Cancer Screening with Professor Fraser Brims
Lung Foundation Australia believes that this media scrutiny and its stigma findings will present a challenge for the screening program because individuals need to disclose their smoking history to be eligible.
Lung Foundation Australia Chief Executive Mark Brooke said he hoped lung cancer patients and people who smoked were treated with more empathy.
“Better communication, education, and advocacy is essential to the success of the [screening program],” he said.
“By normalising lung cancer screening and fostering a supportive public discourse, the program has the potential to save thousands of lives while also reshaping the narrative around lung cancer in Australia.”
Want more news, clinicals, features and guest columns delivered straight to you? Subscribe for free to WA’s only independent magazine for medical practitioners.
Want to submit an article? Email [email protected]

