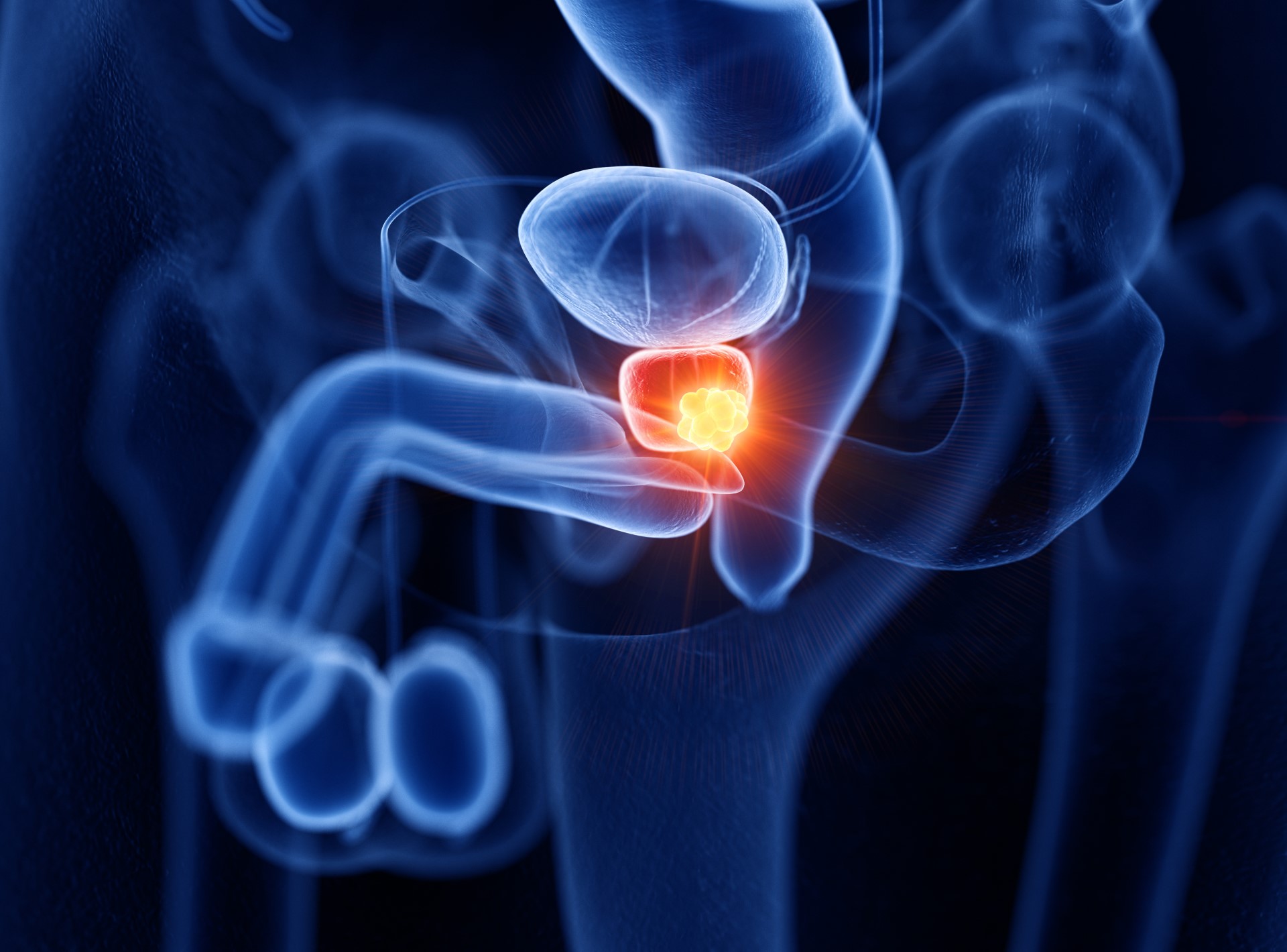
Australian-led research has made a major breakthrough in the diagnosis and detection of prostate cancer, which claims the lives of more than 300,000 men every year.
According to the study, published in Cancer, the international team led by UniSA has identified three new biomarkers for prostate cancer to help pathologists differentiate potentially aggressive cases of the disease.
The biomarkers Appl1, Sortilin, and Syndecan-1, demonstrated greater accuracy when predicting clinical recurrence (CR) and biochemical recurrence (BCR) than the traditional, five-tiered Gleason scoring system, which relies on the accurate grading of hematoxylin and eosin (H&E)-stained tissue sections to guide treatment decisions.
Lead author, UniSA’s Professor of Molecular Medicine Dr Doug Brooks, explained that the new biomarkers were part of the endosome-lysosome system, and immunohistochemistry (IHC) labelling of these proteins “enabled improved visualisation of the complex pathologies underlying prostate cancer.”
“While Gleason/ISUP grade grouping using H&E is validated for predicting biochemical recurrence (BCR) post-surgery, it is well recognised that this method is far from optimal,” he said.
“The interpretation of Gleason grading using H&E is highly subjective, resulting in high inter-observer variability and subsequent sub-optimal treatment selection for many individual patients, and it is anticipated the new biomarkers will lead to long-term improvements in the way prostate cancer is diagnosed and graded. They are remarkably sensitive and specific in accurately visualising the progress of the cancer and confirming its grade.
“This discovery has led to the commercial development of a test designed to determine how advanced and aggressive the cancer is and whether immediate treatment is needed.”
The study was a retrospective assessment of 114 Adelaide men with prostate cancer, who had provided a radical prostatectomy tissue block sample to the Australian Prostate Cancer Bioresource (APCB) between January 2006 and August 2014.
“At the time of radical prostatectomy, these patients were treatment-naïve and had a prostate-specific antigen (PSA) level above 0.2 ng/mL,” the authors said.
“For pre-radical prostatectomy, most patients had a PSA level between 4.5 ng/mL and 22 ng/mL, while a small percentage (7.9%) were lower than 4.5 ng/mL.
“Patients ranged in age from 45–75 years old at radical prostatectomy and had a BMI between 22 and 39, with clinical follow-up on BCR and metastatic disease progression (CR) available for a minimum of 10 years post-surgery.
“At the time of tissue block sampling, data were available on statuses of extracapsular extension, surgical margin, as well as seminal vesicle, perineural and lympho-vascular involvement.”
Recurrence was defined as the time interval from the day of radical prostatectomy to the day of CR.
The tissue samples were graded using an H&E slide and then independently graded using Appl1, Sortilin, and Syndecan-1 IHC-labelled slides, and the comparison revealed that “34 patients (30%) had an increase, and 14 patients (12%) had a decrease in their ISUP grade group with the use of the IHC-labelled slides, as compared to the H&E slide.”
The team from UniSA also collaborated with the Australian company C, which funded the research and has signed a commercialisation contract with the largest pathology provider in the US, Quest Diagnostics, to launch the technology.
“It is expected that clinical trials using the innovative technology will be undertaken in Australia, following its successful implementation within the American healthcare system,” Professor Brooks said.