 A device created and trialed here in Western Australia is being described as the biggest development in the way babies are monitored during birth for half a century.
A device created and trialed here in Western Australia is being described as the biggest development in the way babies are monitored during birth for half a century.
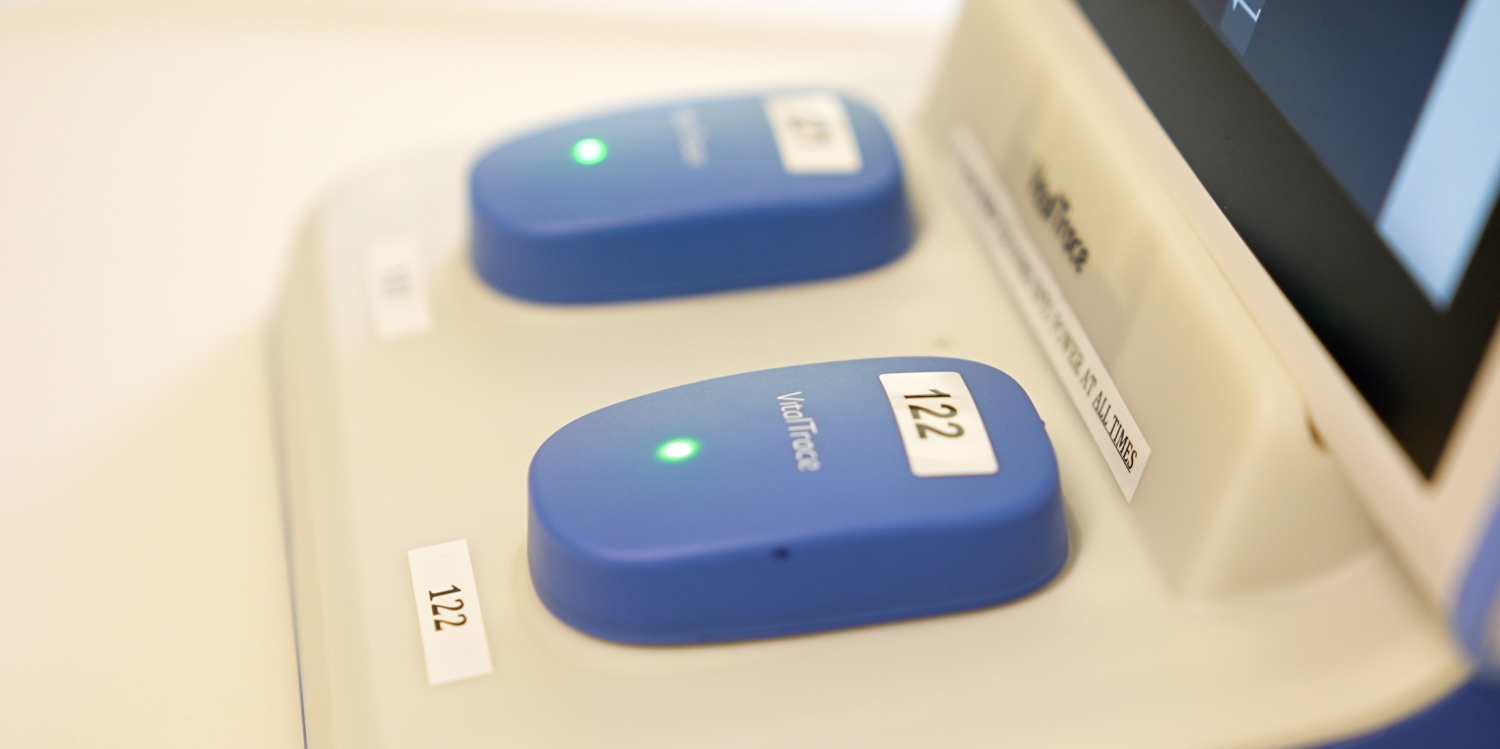
VitalTrace immediately detects when a baby is not receiving enough oxygen during labour and alerts healthcare professionals.
The device has been trialed across four Australian sites, including King Edward Memorial Hospital (KEMH).
WA medtech company VitalTrace partnered with researchers from UWA and the University of Sydney to bring the device to hospitals.
The device detects a lack of oxygen by providing a continuous signal that tells clinicians about the level of lactate in the baby’s blood.
A small electrode sensor is applied by an obstetrician or midwife into the skin of the baby’s scalp once the mother’s waters have broken and the baby’s head is accessible.
The device then transmits information from the sensor to a monitor using wireless technology, which means the mother can move around freely during labour.
Professor Jane Pillow, National Health and Medical Research Council (NHMRC) leadership fellow and senior principal research fellow at UWA’s School of Human Sciences, said the device provided the first major breakthrough in foetal monitoring techniques during labour and birth for more than 50 years.
After extensive preclinical testing, the device was recently applied for the first time to a baby during labour at Sydney’s Royal North Shore Hospital as part of the world-first clinical trial. The trial is also underway at KEMH and at Melbourne’s Monash Health and Box Hill Hospital.
RELATED: Private maternity and obstetrics in the spotlight
So far, nine women and their babies have participated in the study.
VitalTrace co-founder and chief executivr Dr Arjun Kaushik, a UWA medicine graduate, said this new device enabled clinicians to continuously monitor babies and their levels of oxygenation during labour.
“This real-time feedback means that, for the first time, health practitioners caring for a woman in labour will be able to detect immediately when a baby is not receiving enough oxygen to the brain,” Dr Kaushik said.

Dr Kaushik said current methods that measured the baby’s heart rate during labour had the tendency to be very inaccurate, which resulted in missed diagnosis of foetal brain injury and unnecessary rates of intervention, such as caesarean sections.
The device also has the potential to prevent major health issues, such as birth asphyxia and cerebral palsy.
Dr Kaushik said women who had experienced foetal monitoring while giving birth had provided extensive and valuable input into the research, which influenced the design of the invention.
The State Government’s Future Health Research and Innovation Fund supported the project in its early stage, providing the capital needed for UWA to transform the initial idea into a viable product.
Medical Research Minister Stephen Dawson congratulated those involved in designing the device and said he was looking forward to seeing this WA innovation used routinely in patient care.
Want more news, clinicals, features and guest columns delivered straight to you? Subscribe for free to WA’s only independent magazine for medical practitioners.
Want to submit an article? Email [email protected]

