Obstructive sleep apnoea (OSA) and resultant sleep fragmentation and oxygen desaturation have been associated with daytime sleepiness, cognitive impairment, Type 2 diabetes, cardiovascular disease, stroke, increased risk of motor vehicle accidents and can have significant effects on quality of life. It can affect 4% to 9% of the middle-aged population (up to 34% of men in some studies) and is two to three times more common in older individuals than those under 64 years.

Sufferers require an effective and long-term treatment. The gold standard is to pneumatically splint the upper airway during sleep using continuous positive airway pressure (CPAP). Whilst highly efficacious in preventing upper airway collapse, providing a successful outcome in over 95% of users, as many as 50% of patients cannot tolerate CPAP treatment.
Many look to alternative treatment options such as a mandibular advancement device (MAD) of which there are numerous types.
Generally MAD aims to create a widening of the upper airway configuration by posturing the mandible forward. This action changes the dimensions of the upper airway, including the hypopharynx, the oropharynx, and the nasopharynx. Imaging studies have shown the upper airway space expands, most notably in the lateral dimension of the velopharyngeal region.
MADs is hypothesised to increase muscular tonus by increasing passive muscle tension in the pharyngeal wall, thereby reducing soft tissue vibration and the turbulent airflow.
The clinical practice guideline of the American Academy of Sleep Medicine (AASM) and American Academy of Dental Sleep Medicine (AADSM) recommends that adult patients without OSA requesting treatment of primary snoring be prescribed oral appliances, rather than no therapy. For adults with OSA, both oral appliances and CPAP can significantly reduce the apnoea-hypopnea index/respiratory disturbance index/respiratory event index (AHI/RDI/REI) across all levels of OSA severity in adult patients.
CPAP remains first line therapy for the treatment of adult patients with severe OSA. However, it is recommended that those intolerants of CPAP therapy or preferring alternate therapy be provided with an oral appliance, rather than no treatment.
MAD use may be more acceptable than CPAP for patients with chronically impaired nasal ventilation or frequent travellers (preferring the convenience of a MAD). Consultation with the patient’s sleep physician is appropriate.
When oral appliance therapy is prescribed by a sleep physician, a qualified dentist who has further training in the area should construct a custom, titratable appliance over a non-custom oral device. Periodic review by the qualified dentist is important for dental related-side effects, including bite (occlusal) changes.
Potential side effects of a MAD include excessive salivation, dry mouth and pain or discomfort in the supporting teeth, oral mucosa, masticatory muscle and temporomandibular joint disorders (TMJD). They have been reported as temporary side effects during short and medium periods of oral appliance use. Mostly these side effects are transient and often treatable.
Long-term side effects include occlusal changes, most often without the presence of pain. In a few patients, persistent TMJD may result in discontinuation of MAD therapy.
Other considerations before providing a MAD include the need to exclude active periodontal and dental disease, the amount of mandibular protrusion achievable by the patient, presence of mandibular teeth, dental wear, dentures or mouth breathing, patient preference, and potential for future combination therapy.
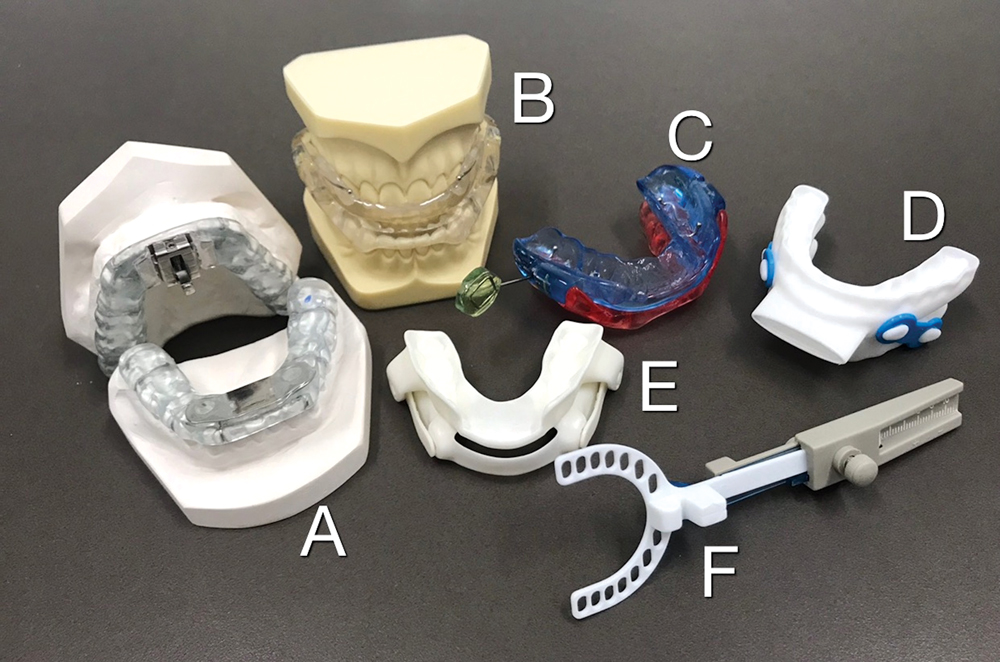
Broadly, the most common MAD devices may be classified as unconnected, those with front connectors, those with side connectors (Image D), tongue retaining devices and other. Nylon 3D printed MADs (Image E) are increasingly being used with good effect and are felt to be more comfortable that traditional acrylic devices (Image B, C). Bruxers may benefit from a MDSA device (front connector, Image A) which allows for side-to-side movements of the mandible often seen in bruxism. Edentulous patients may be suitable for a tongue retaining device.
Key messages
- A mandibular advancement device may be used to treat OSA
- When oral appliance therapy is prescribed by a sleep physician, a qualified dentist should construct a custom, titratable appliance
- Periodic review is important to monitor for side effects.
Author competing interests – nil

