 A 75-year-old man presented with severe impairment of his general condition. On physical examination, stiffened ear cartilage compatible with petrified ears was noticed.
A 75-year-old man presented with severe impairment of his general condition. On physical examination, stiffened ear cartilage compatible with petrified ears was noticed.
Challenge
A 75-year-old man presented with severe impairment of his general condition and progressive cachexia requiring enteral nutrition via tube. Serum calcium was normal, whereas sodium was low. On physical examination, stiffened ear cartilage compatible with petrified ears was noticed. A 3D reconstruction from a CT scan confirmed calcification of the elastic cartilage of both external ears.
What is the most likely diagnosis?
- Systemic scleroderma
- Adrenal insufficiency
- Calciphylaxis
- Hyperparathyroidism
Background
A 75-year-old man was admitted to our Department of Endocrinology with a 2-month history of recurrent pneumonia, somnolence, and progressive cachexia requiring enteral nutrition via a percutaneous endoscopic gastrostomy tube.
On inspection, his ears appeared normal, but on palpation they were found to have a stone-like hardness. An x-ray (figure, A) and a 3D reconstruction from a CT scan (figure, B) showed ossification of the auricular cartilage, including helix, antihelix, and antitragus. There were no other manifestations of pathological ossification.
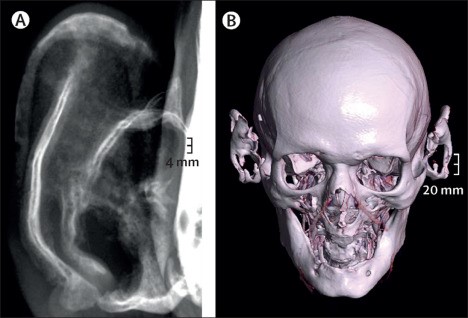
Figure. X-ray and CT findings from a 75-year-old man with secondary adrenal insufficiency. (A) X-ray image of the patient’s right auricular helix, antihelix, and antitragus. (B) 3D reconstruction from a CT scan showing calcification of the auricular cartilage.
His wife reported that the man had had recurrent episodes of weakness during stressful situations over the past 20 years. Clinical examination of the patient revealed somnolence, hypotension (blood pressure <100/60 mm Hg), and cachexia (weight 50 kg, height 174 cm, BMI 16·5 kg/m2). Laboratory analysis showed hyponatraemia (serum sodium 124 mmol/L [reference 136–145 mmol/L]) and concomitant borderline hyperkalaemia (serum potassium 4·94 mmol/L [reference 3·40–4·40 mmol/L]).
What is the most likely diagnosis?
- Systemic scleroderma
- Adrenal insufficiency
- Calciphylaxis
- Hyperparathyroidism
Breakdown
Low morning serum cortisol (123 nmol/L [reference 133–537 nmol/L between 0600 h and 1000 h]) and low adrenocorticotropic hormone (2·06 ng/L [reference 7·2–63·3 ng/L between 0600 h and 1000 h]) and negative results for adrenal autoantibodies confirmed secondary adrenal insufficiency.
Glucocorticoid and mineralocorticoid replacement was initiated, and the clinical condition of the patient improved rapidly. Additional diagnostic tests showed insufficiency of the gonadotropic axis, but the thyrotropic and somatotropic axes were intact. However, a MRI scan of the sella did not reveal any specific cause of partial hypopituitarism. No other endocrinopathies or diabetes were detected. The patient also reported painless stiffness of both ears over the past 10 years.
Rheumatological and immunological work-up showed no remarkable findings, nor was there a history of frostbite or traumatic brain injury. Pathological calcification and, even more rarely, ossification can occur on a background of dystrophic calcification or Albright hereditary osteodystrophy and fibrodysplasia ossificans. Endocrinopathies (eg, adrenal insufficiency, hypothyroidism, and acromegaly), metabolic disease (eg, diabetes), mechanical or hypothermic trauma, and inflammatory disease (eg, perichondritis and systemic chondromalacia) have been reported to be associated with petrified ears. However, to date, the underlying mechanisms remain unclear and no treatment is currently available to reverse calcification or ossification.
At the 1-month follow-up visit after discharge from hospital, the patient had responded well to regular glucocorticoid replacement. His weight had increased to 55 kg and the percutaneous endoscopic gastrostomy tube could be removed. However, both ears remained petrified. Despite being a rare occurrence, petrified ears can be diagnosed easily during physical examination and might suggest long-term clinical or subclinical adrenal insufficiency.
More details
- Original story: Petrifying: ears as hard as stone in adrenal insufficiency (The Lancet D&E)
- Authors: Swantje Kannenberg, MD; Svenja Meyhöfer, MD; Prof Hendrik Lehnert, MD; Prof Sebastian M Schmid, MD.
- All content for this article belongs to The Lancet D&E. For more case examples, visit the Picture Quiz Gallery.

