In general practice, primary hyperparathyroidism may occur as commonly as one in 2000 patients. This disorder is characterised by an elevated serum calcium, an elevated or inappropriately normal serum PTH, and frequently low serum phosphate due to renal phosphate wasting.

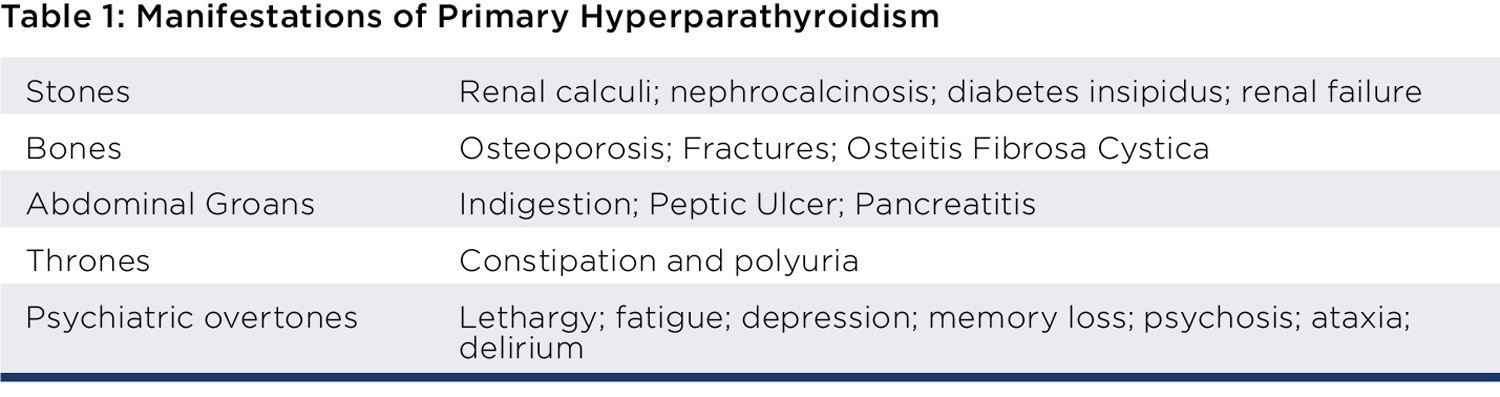
The signs and symptoms of primary hyperparathyroidism are classically summarised by “stones, bones, abdominal groans, thrones and psychiatric overtones”. These manifestations reflect end organ damage as illustrated in Table 1. In today’s practice, most patients are asymptomatic, and are identified on routine biochemistry, or during investigation for secondary causes of osteoporosis. Many patients may have subtle symptoms of fatigue and weakness that resolve after parathyroidectomy.
The key to patient management is having a clear and unequivocal biochemical diagnosis. Should there be any doubt with regards to the biochemistry, then performing a fasting metabolic bone study (a consolidated serum and urine assay) is usually diagnostic.
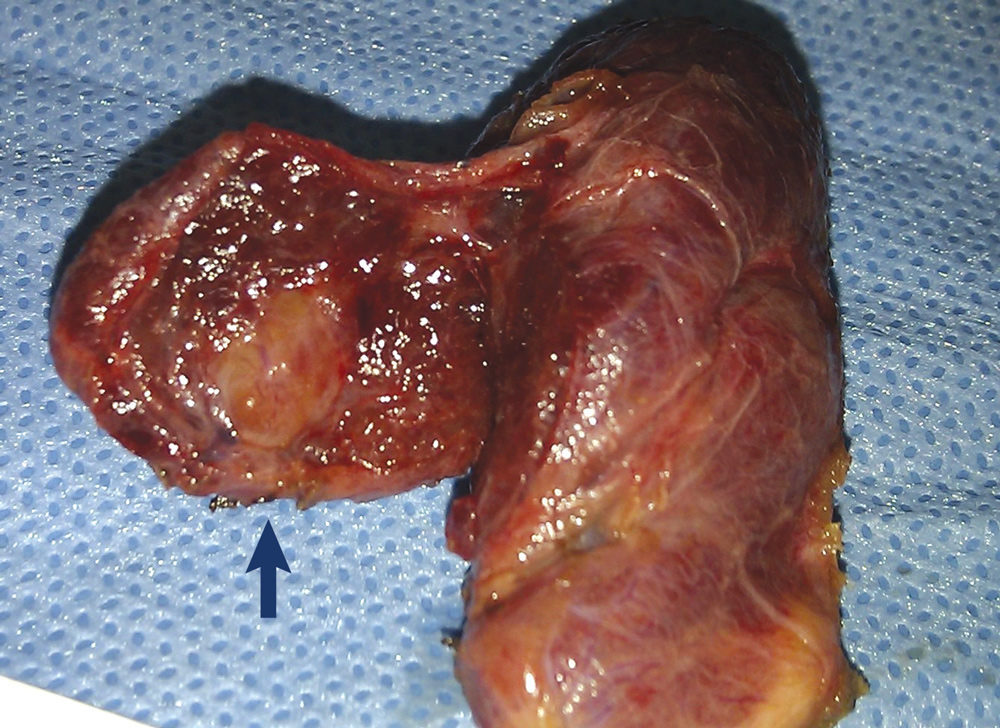
In 85% of patients with primary hyperparathyroidism, the cause is a single parathyroid adenoma. The remaining 15% of patients have multiglandular disease. Surgical removal of the offending parathyroid gland (or glands) is generally curative. The reason parathyroidectomy is only curative in over 98% patients with one procedure, is due to the occasional ectopic parathyroid adenoma which can be challenging to find.

Parathyroidectomy is indicated for all symptomatic patients, should be considered for most asymptomatic patients, and is more cost-effective than observation or pharmacologic therapy.
Symptomatic patients are expected to derive clear benefits from curative parathyroidectomy, and patients considered to be asymptomatic frequently report improvement in quality-of-life indexes. Long-term hypercalcemia should be avoided because of potential end organ damage. Surgeons who regularly perform parathyroidectomy should have a complication rate of under 1%.
Imaging and localisation
The key indication for surgery is a concrete diagnosis and patient fitness for surgery. Many imaging modalities are available to assist with surgical planning and to provide the patient with differing surgical options.
However, the most important imaging modality prior to surgery would likely be neck ultrasound. The key role of preoperative neck ultrasound is to exclude, or evaluate, any underlying incidental thyroid lesions prior to neck surgery.
One of the guiding principles in thyroid and parathyroid surgery is to try to perform any surgery only once. The reason is that re-operative neck surgery does carry a higher risk of morbidity. Therefore, it would be prudent to be aware of any incidental thyroid lesions so that if thyroidectomy is indicated, this is also performed at the same procedure. Additionally, ultrasound performs moderately well in identifying parathyroid adenomas.
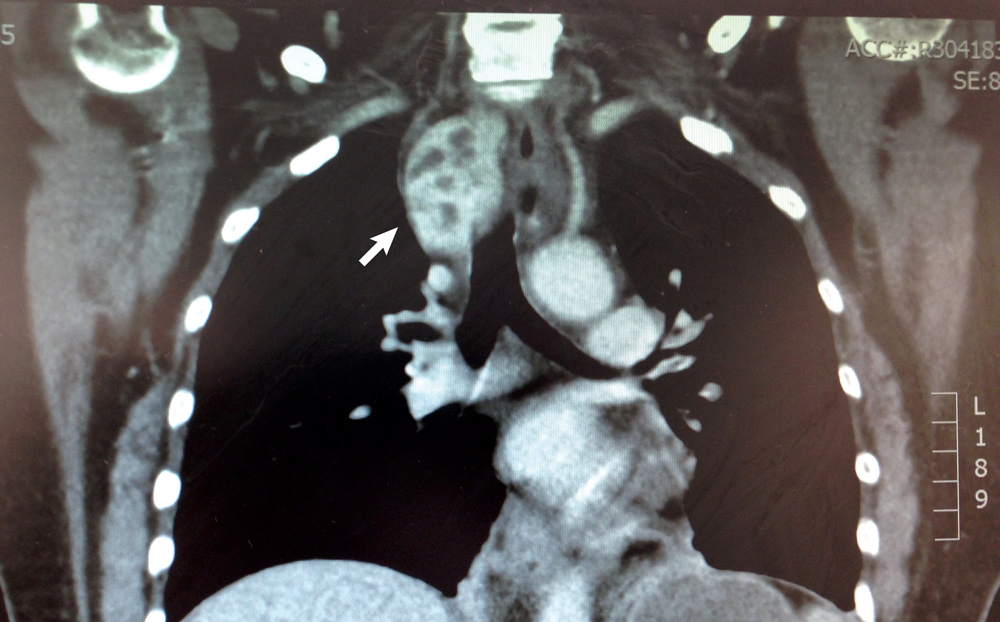
Parathyroid localisation studies attempt to identify the diseased parathyroid gland/glands. Commonly available localisation studies include 4D CT / parathyroid CT scan; and sestamibi scan. Unfortunately, none of these scans are perfect. They are operator dependent, roughly 30% of scans are not able to localise, and even when successful localisation occurs, false positives do occur in roughly 10% of patients.
However, a positive localisation study does allow the patient to have a more focused, minimally invasive operation, which is reflected in either a smaller neck incision or a scarless transoral endoscopic approach.
 Postoperative care
Postoperative care
Parathyroidectomy in the hands of an experienced parathyroid surgeon has a very high success rate for cure and very low potential for morbidity. Prospectively collected audit results of our local West Australian tertiary hospital endocrine surgeons demonstrates complication rates of under 1%.
For confirmation of cure, serum calcium and parathyroid hormone assays should be performed six and 12 months after surgery. The key indicator for cure is maintenance of eucalcaemia. Serum Parathyroid hormone levels can sometimes be elevated in the presence of eucalcaemia. This phenomenon may occur in about 20% of patients. This likely relates to a degree of vitamin D or calcium deficiency.
Vitamin D and calcium supplementation may be useful and annual repeat serum calcium and parathyroid assays would be worthwhile if abnormalities persist. A subgroup of these patients may develop multiglandular parathyroid disease on long-term follow up, which may necessitate subsequent careful evaluation, and possible further intervention.
Key messages
- Unequivocal biochemical diagnosis is key
- Primary hyperparathyroidism is curative in the majority of suitable surgical candidates
- Evaluation and management by an experienced parathyroid surgeon is critical.
– References available on request
Author competing interests – nil

