 Prenatal screening is becoming more complex as technology expands the number of disorders potentially diagnosable prior to birth and as screening evolves to incorporate expanded genetic carrier screening and rarer chromosomal malformations.
Prenatal screening is becoming more complex as technology expands the number of disorders potentially diagnosable prior to birth and as screening evolves to incorporate expanded genetic carrier screening and rarer chromosomal malformations.
The options can be overwhelming for health care providers and women, potentially overshadowing the joy of pregnancy if not approached in a reasoned manner. Support and advice from trained genetic counsellors and specialists in prenatal diagnosis should be actively sourced when needed.

Current obstetric practice guidelines in Australia advocate offering prenatal screening for fetal structural and genetic abnormalities, with the final decision for testing residing with the woman.
The test performance characteristics of non-invasive prenatal testing (NIPT) for the common fetal aneuploidies are superior to combined First Trimester Screening (cFTS), although the expansion of NIPT into sex chromosome aneuploidy and microdeletion screening is associated with substantial false positive rates.
Non-invasive prenatal testing has resulted in a significant reduction in amniocentesis and CVS. However, this reduction may be reversed if expanded NIPT panels become more widely used.
Without a national policy, two main strategies have evolved for non-invasive prenatal testing – to offer it as a first line test or after an increased risk cFTS.
Non-invasive prenatal testing is not considered diagnostic for trisomy 21, 13 or 18. An increased probability result should be confirmed by a diagnostic test (e.g. CVS or amniocentesis). Sensitivity is lower in twin pregnancies.
If non-invasive prenatal testing as a primary screen returns an increased probability for trisomy 13 or 18 but the fetus appears unremarkable to expert ultrasound, an amniocentesis (not CVS) is indicated to sample the fetal karyotype.
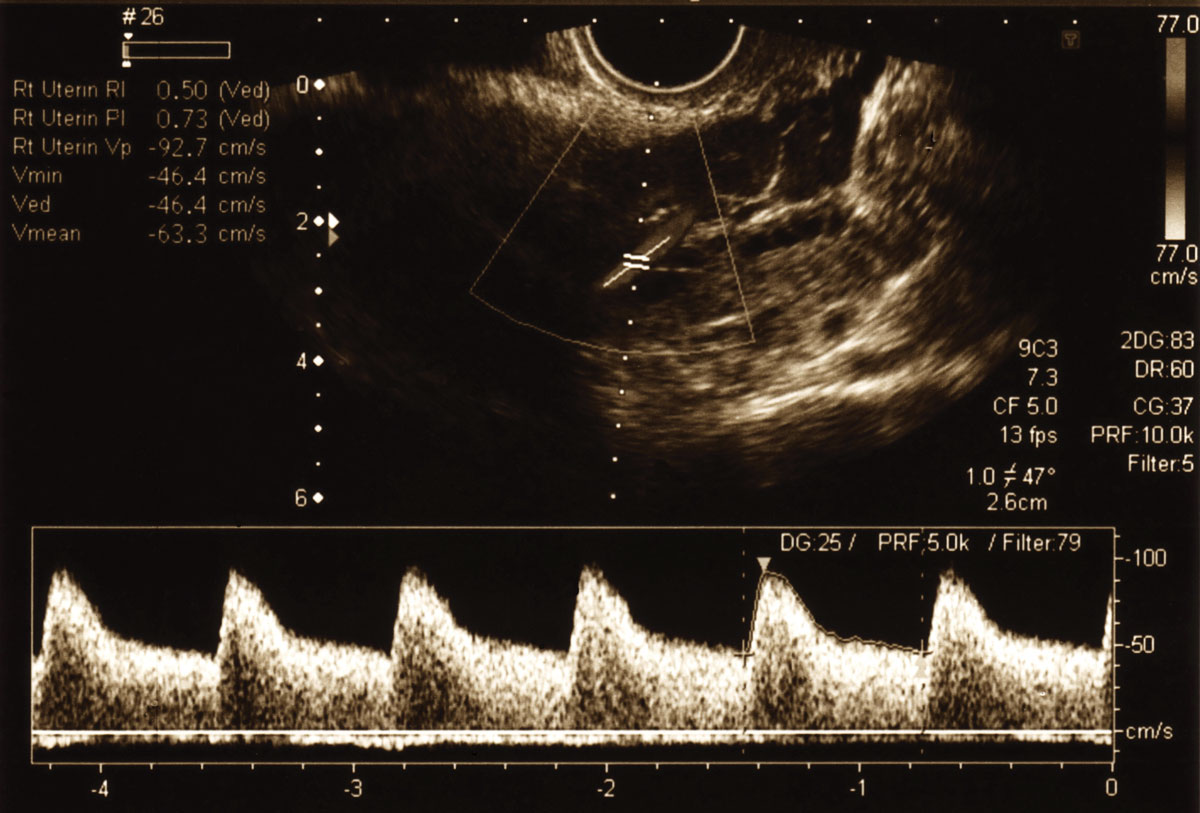
If a cFTS demonstrates a large nuchal translucency (>3.5-4 mm), if the fetus displays structural malformations or if the cFTS result is >1:20 – NIPT is not an appropriate next step. Referral for advanced imaging and a diagnostic genetic test is required.
In 1-3%, non-invasive prenatal testing fails to provide a result (‘no-call’). This is usually due to a low fetal cell-free DNA fraction (which can be associated with factors like maternal obesity) or laboratory technical issues. Other reasons include fetal chromosomal abnormalities, maternal autoimmune disease or maternal heparin use. In the situation of a no-call result, a repeat non-invasive prenatal testing should be offered, but consider referral for expert ultrasound review.
Maternal chromosomal abnormalities, malignancies, recent blood transfusion and solid organ transplantation may produce difficulties in the interpretation of NIPT.
Advanced non-invasive prenatal testing is now available in the form of genome-wide (GW) cfDNA NIPT; with no additional cost, and no delay in turnaround time (3-5 working days). Genome-wide NIPT reports on extra or missing whole chromosomes across all chromosomes, rare autosomal aneuploidies, copy number variations (CNVs) including duplication and deletions, and unbalanced translocations.
 Rare autosomal aneuploidies (RAAS) are the monosomies and trisomies not restricted to chromosomes 13, 18, 21 and frequently represent confined placental mosaicism (CPM) (e.g. trisomy 7). Identifying RAAS early in an ongoing pregnancy may assist in guiding management through the use of serial ultrasound to monitor for IUGR (although there is variance of opinion about this issue).
Rare autosomal aneuploidies (RAAS) are the monosomies and trisomies not restricted to chromosomes 13, 18, 21 and frequently represent confined placental mosaicism (CPM) (e.g. trisomy 7). Identifying RAAS early in an ongoing pregnancy may assist in guiding management through the use of serial ultrasound to monitor for IUGR (although there is variance of opinion about this issue).
Prenatal diagnosis via amniocentesis is required to identify true fetal mosaicism (TFM) and/or potential UPD if imprinting chromosomes are involved
CNV include deletions, duplications, unbalanced translocations and other complex changes which are screened for across all autosomes (excluding the sex chromosomes), with or without a family or personal history. One in 500 individuals carry a balanced reciprocal translocation and can experience subfertility, recurrent miscarriage, fetal loss or the birth of a baby with a severe disability. Most familial translocations are unique and occur across all chromosomes.
Couples who are balanced translocation carriers, and/or have experienced a fetal CNV in pregnancy (de novo or familial), report heightened anxiety in subsequent pregnancies. Many couples want an alternative to invasive testing, especially if they have a history of multiple miscarriage.
A low probability screening result can provide early reassurance. A high probability screening result guides the appropriate use of diagnostic testing
Genome wide non-invasive prenatal testing provides most translocation carriers with a non-invasive screening option for their specific, and often unique chromosomal arrangement. It is an option for couples with prior fetal de novo duplication or deletion and low risk of recurrence but heightened anxiety. It provides information to assist decision making regarding invasive diagnostic testing following a low or a high probability screening result.
Early detection for rare aneuploidies may have implications for pregnancy and fetal wellbeing. For many it is an option for early and safe reassurance, altering the path and early bonding experience of a pregnancy, especially after previous fetal loss or infertility.
Key messages:
- Non-invasive prenatal testing is a sensitive and specific screening test for the detection of trisomy 21, 18 & 13, but less so for other chromosomal malformations
- A fetal abnormality on ultrasound should, in most cases, be regarded as a contraindication to non-invasive prenatal testing
- A no-call result on non-invasive prenatal testing may be the first indicator of increased obstetric risk
References available on request.
Questions? Contact the editor.
Author competing interests: None to disclose.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.


