 For many Australian men with low-risk prostate cancer, treatment options are not being clearly laid out, and many may be getting unnecessary surgery.
For many Australian men with low-risk prostate cancer, treatment options are not being clearly laid out, and many may be getting unnecessary surgery.
GPs and other health care providers should carefully consider if a low-risk prostate cancer patient really needs to undergo surgery.
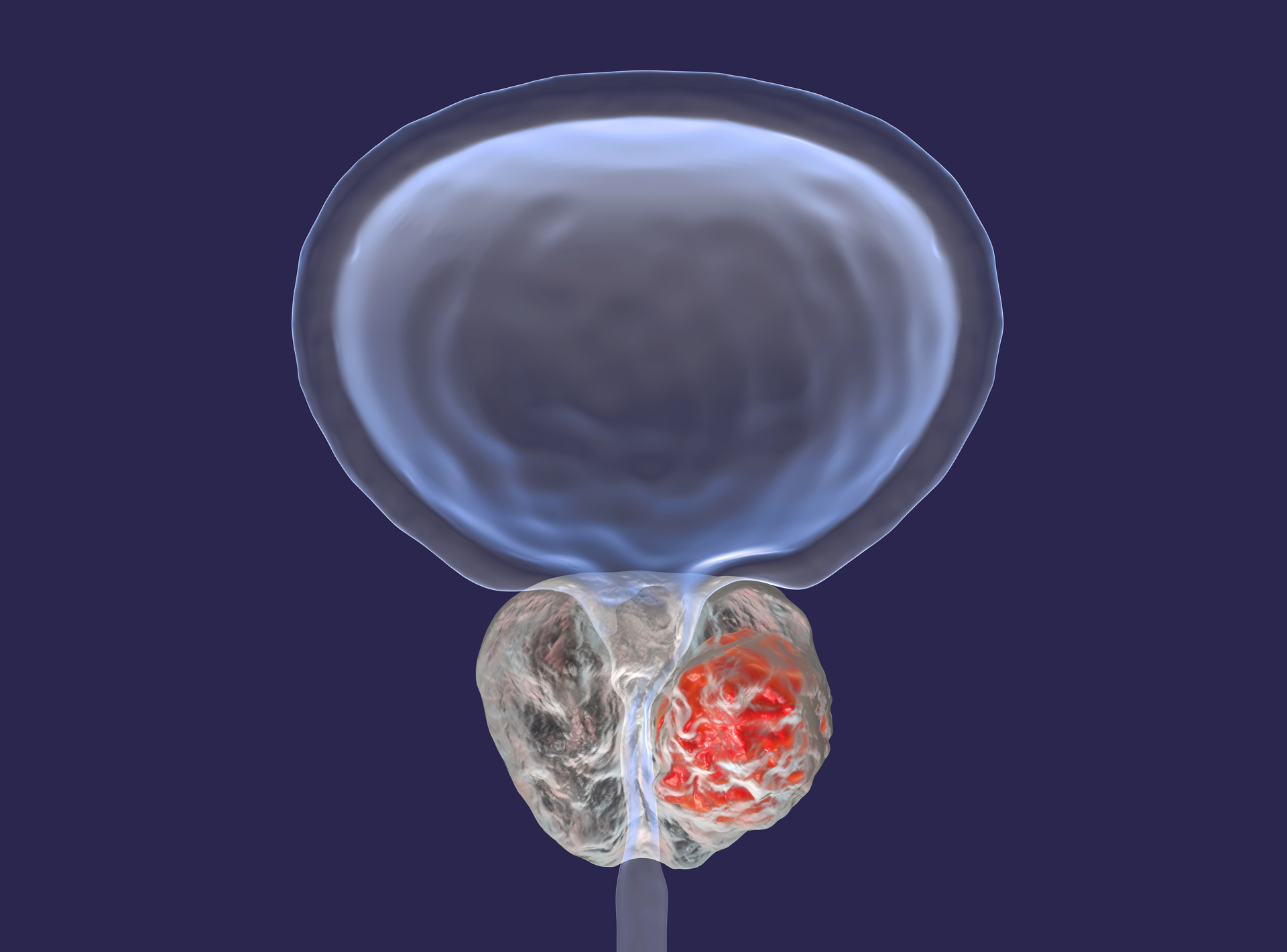
Prostate cancer is the most common cancer diagnosed in Australian men, with 16,741 cases diagnosed in 2020. While different treatment options are available, including surgery, radiotherapy, and active surveillance, the survival rates for each of these treatments is roughly the same. However, there are significant differences in terms of side effects associated with each of these treatments. For example, following surgery men often experience urinary incontinence and erectile dysfunction, among other problems.
There are also significant differences in the way prostate cancer patients are managed and in the information they receive about treatment options available.
A recent study in the Medical Journal of Australia, found that, among 4003 New South Wales men in the 45 and Up Study who were diagnosed with prostate cancer, 40% received radical surgery to remove their prostate gland compared with only 22% who received radiotherapy and 21% who received no active treatment. Furthermore, the study also found that only 13% of the men receiving surgery consulted a radiation oncologist before “going under the knife”.
The study also identified certain factors associated with a higher likelihood of receiving surgery. For example, men who were more likely to receive surgery were aged 45‒59 years, with regional stage disease, living 100 km or more from the nearest radiotherapy centre, having partners, or having private health insurance.
“Our study found that patients living in more advantaged areas or those who had private health insurance were more likely to receive prostate surgery than radiotherapy. This suggests that patients do not have equitable access to care, with the ability to afford private health insurance and the associated out-of-pocket costs influencing the type of treatment received,” said Dr Mei Ling Yap, radiation oncologist and conjoint senior lecturer at the Collaboration for Cancer Outcomes, Research and Evaluation (CCORE), Ingham Institute, UNSW Sydney, Australia
The findings suggest that, for some patients, there is a significant bias in favour of receiving surgery, compared to other treatment options.
“A key finding of our study was that fewer than 1 in 7 men diagnosed with prostate cancer saw a radiation oncologist for an opinion on management prior to undergoing surgery. This means that men with prostate cancer are not receiving information about their management options from all appropriate specialists,” Dr Yap said.
While this lack of information about treatment options results in virtually the same survival outcomes, there are other important outcomes that are significantly affected, Dr Yap explains, like side effects and financial costs associated with each treatment. “Ensuring patients are fully informed about all management options will empower men with prostate cancer to make the decision that is most likely to lead to the best quality of life for them,” she said.
While surgery and radiotherapy are part of the standard of care, for many patients, no treatment at all, commonly known as active surveillance, may be a viable option – and one that results in the best health outcomes.
Active Surveillance
It is estimated that as many as 70% of men with low volume, low risk prostate cancer will not require any intervention for at least 5 years, as concluded in this report. Instead, patients are closely monitored and tested regularly for cancer growth. Prostate cancer patients managed with active surveillance should expect to receive regular testing, including blood tests for Prostate-specific antigen (PSA), Digital Rectal Examinations, MRI scans, and biopsies.
But apart from the hassle of regular testing, choosing active surveillance may result in a high quality of life for many patients, with the side effects associated with surgery or radiotherapy avoided or delayed– and is also associated with high survival rates.
Patients with newly diagnosed prostate cancer should discuss all their treatment options with their GP and their relevant specialists to ensure they are well informed and that the best treatment option is selected according to their disease type, age, other health factors and their personal preferences.
“An increase in the uptake of joint uro-oncology clinics, where prostate cancer patients are seen by both urologists and radiation oncologists at the same appointment, would help to ensure that patients are seen by all relevant specialists prior to undergoing treatment,” Dr Yap said.
In addition, it would be ideal if all management options for prostate and other types of cancer would be freely available through public health care, Dr Yap explains, without any out-of-pocket expenses for patients. This would result in all patients having equitable access to health care. “Lastly, advocacy and education programs are needed to ensure that patients, their partners and caregivers, and their physicians are fully informed about all treatment options,” Dr Yap added.

