 Traditionally, conditions such as Osgood-Schlatter’s Disease (OSD) and Severs Disease have been described as self-limiting, as an apophysitis not negatively affecting growth, and thought to resolve on growth plate closure. However, this is not what we are seeing in clinics and research.
Traditionally, conditions such as Osgood-Schlatter’s Disease (OSD) and Severs Disease have been described as self-limiting, as an apophysitis not negatively affecting growth, and thought to resolve on growth plate closure. However, this is not what we are seeing in clinics and research.

In one perspective cohort study of adolescents with OSD, even at two years after diagnosis, 60% demonstrated persistent tendon changes. Research through Aalborg University showed at two years, 40% report continued OSD related pain, and although severity was variable, these adolescents were impeded in sports participation and recorded lower quality of life. Severs can also have a tangible negative effect on quality of life.
Why should we re-examine our management of apophysitis? Adolescence is a key developmental period where the apophysis changes to a mature enthesis. It is a critical time for the formation of normal tendon attachment. It is possible that overly aggressive sporting activity and tendon loading during symptomatic OSD may (long term) negatively impact both tendon structure and the risk of adulthood symptoms.
Prof Jens Olesen, a rheumatologist and sports physician at Aalborg University, found those patients with OSD whose initial ultrasound showed a combination of fragmentation of the tibial tuberosity ossification centre, thickening of the patellar tendon insertion and infrapatellar bursitis were more likely to continue to experience persistent pain and dysfunction.
With improved understanding of the long-term effects on participation and quality of life, these conditions should be treated efficiently and effectively. Active management of the condition is appropriate, rather than simply asking them to cease sporting activities until cessation of symptoms, as past literature suggests.
As health practitioners we are efficient at addressing acute pain management through ice, taping, analgesics and deloading. However, are we supporting full return to activities? What else can we do?
Plenty.
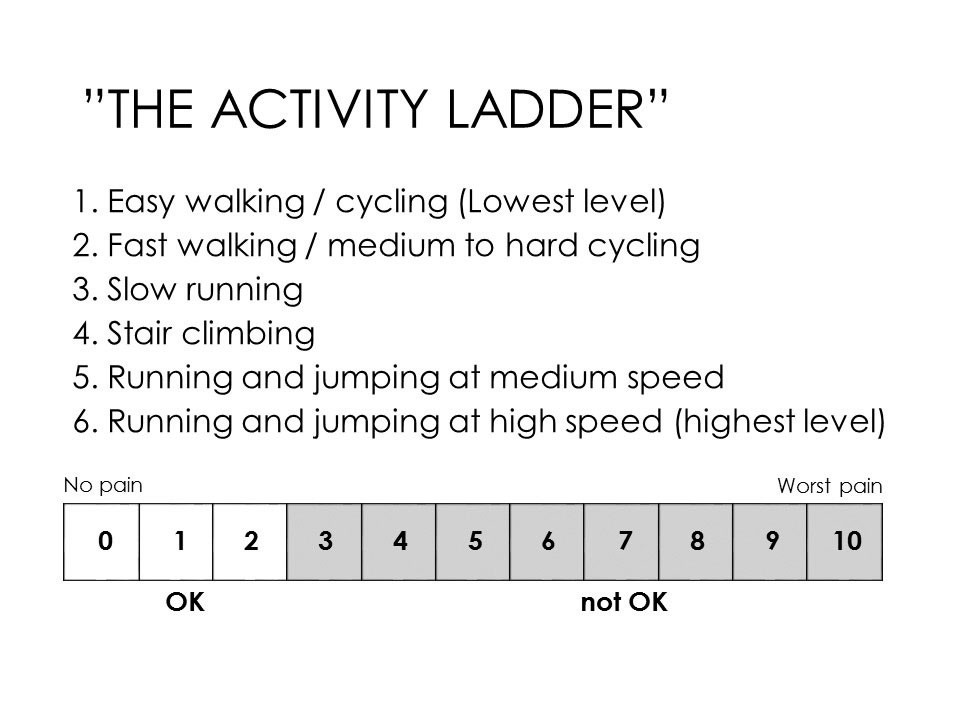
Load modification is the mainstay of treatment. Increased practice time has been shown to be a risk factor for OSD onset. Thus, the basic approach is activity modification; deloading is required and using a tool such as the Activity Ladder (Fig 1.) to quantify and accurately progress loads is improving clinical practice.
Factors such has higher mean BMIs, deficits in muscle strength, reduced jumping ability, reduced flexibility, reduced shock absorption and altered biomechanics can all be addressed to reduce symptoms and improve function. For calcaneal apophysitis, the use of heel raises or orthoses can provide short-term pain relief and improved participation.
The days of the passive “wait and see” and “rest is best” approach have gone. Addressing individual deficits and graded loading is an important part of rehab and return to play. Early intervention and appropriate referral are key.
Key messages
- Growing pains can negatively impact quality of life
- Structural changes may persist into adulthood
- Manage actively rather than “wait and see”
References available on request.
Questions? Contact the editor.
Author competing interests: nil relevant disclosures.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

