This content is part of a paid partnership with Australian Clinicallabs.

Head and neck tumours are common in the adult population, with major attention paid to epithelial malignancies given the significant morbidity and mortality associated with these pathologies. In infants, adolescents and young patients, however, soft tissue tumours are more likely to be encountered compared to epithelial malignancies.

Oral Physician & Maxillofacial Pathologist, Nedlands
BDSc, MDSc (OralMed OralPath), PhD, GCEd (HE), GCExLead, MBA, MAICD, AFCHSM, CHM, FRACDS (OralMed), FOMAA, FIAOO, FICD, FPFA, FAIM
Prof Farah is a Consultant Oral & Maxillofacial Pathologist at Australian
Clinical Labs. He is a dual registered specialist in oral medicine and oral
pathology with sub-specialty training in oral oncology. In addition to private practice at Hollywood Medical Centre, he is Consultant in Oral Medicine at
Fiona Stanley Hospital.

by Mr Rob Wormald.
Soft tissue tumours share overlapping clinical presentation, histogenesis and pathological profiles making definitive diagnosis difficult and nuanced. Given the age and growth profile of affected patients, in addition to the invasiveness of treatment approaches, it is important to achieve a correct definitive diagnosis.
In many instances this is not possible on routine haematoxylin and eosin staining of incisional biopsy samples. In such circumstances, immunohistochemical staining for specific markers can help reveal the cell of origin of a particular tumour, with implications for appropriate therapy. An example of this approach is highlighted in the case below.
A 12-year-old female presented with a recent history of an intraoral lump. Clinically the patient presented with an asymptomatic raised 1.5cm firm submucosal nodule visible from the dorsal aspect of tongue, with normal appearing intact overlying mucosa (Fig 1). Clinical differential diagnosis included a granular cell tumour, schwannoma, or other mesenchymal soft tissue tumour.
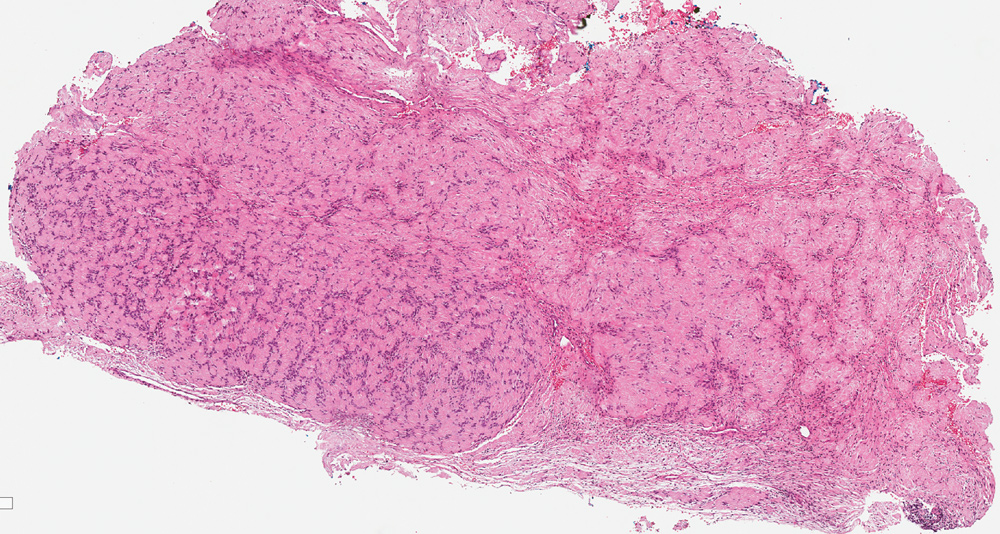
Histopathological examination of a biopsy from the lump showed a circumscribed, unencapsulated, submucosal mass displaying a biphasic hypocellular/hypercellular spindle cell proliferation. The hypercellular region displayed amorphous-looking, eosinophilic material between parallel groups of nuclei, suggestive of Verocay bodies, but lacking typical nuclear palisading (Fig 2). Histopathological differential diagnosis included schwannoma, myofibroblastoma or myofibroma.
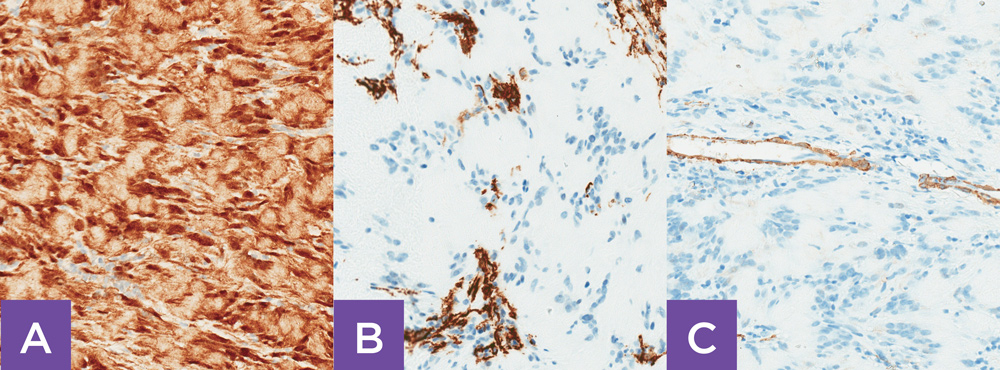
In this example, despite the presence of histopathological features of each of myofibroma, myofibroblastoma and schwannoma on routine haematoxylin and eosin stain, immunohistochemical staining revealed that the lingual tumour was of Schwann cell, and not of myofibroblastic origin (Fig 3), rendering a final definitive diagnosis of Schwannoma. Schwannoma is treated with local resection, with minimal to no evidence of malignant transformation.
Key messages
- Tumours and tumour-like lesions of the head and neck are commonly encountered in medical practice.
- Presentation of a mass in the head and neck should be evaluated with care and examined in detail.
- Soft tissue mesenchymal tumours are more likely to be encountered in infants, adolescents and younger patients.
- Soft tissue tumours share overlapping clinical presentation, histogenesis, and pathological profiles making definitive diagnosis difficult and nuanced.
- Definitive diagnosis often requires immunohistochemical assessment of an adequate tissue sample and expert pathological interpretation.
– References available on request
Author competing interests – the author is an oral and maxillofacial pathologist at Australian Clinical Labs and has written a book on the topic.
Questions? Contact the editor.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website

