 The 12th conference of the International AIDS Society being held in Sydney this week heard the best of news.
The 12th conference of the International AIDS Society being held in Sydney this week heard the best of news.
Professor Andrew Grulich of the Kirby Institute at the UNSW presented findings that Inner Sydney had reduced new HIV acquisitions by 88%, meaning it may be the first locality in the world to reach the UN target to end AIDS as a public health threat by 2030.
Prof Grulich attributed success in Inner Sydney in part to community outreach and prevention efforts, including widespread availability and use of HIV pre-exposure prophylaxis (PrEP).
The announcement comes just one week after the Kirby Institute released national surveillance data showing that new diagnoses of HIV among gay and bisexual men in Australia had fallen by 57% over the past decade.
“The extraordinary success in HIV prevention in the gay neighbourhoods of Sydney is due to decades of government leadership,” Grulich said. “Working in partnership with community and clinical organisations, effective research-based interventions have been designed and implemented. These numbers show us that virtual elimination of HIV transmissions is possible. Now, we need to look closely at what has worked in Sydney and adapt it for other cities and regions across Australia,” he told the conference.
Sharon Lewin, IAS President, and Director of the Peter Doherty Institute for Infection and Immunity at the University of Melbourne, added that “a durable end to Australia’s HIV epidemic requires a cure and a vaccine, and the scientific community won’t stop until we discover them.”
However, the study authors point out that continued success is not guaranteed.
“As Australia stays on course to become one of the first countries to virtually eliminate HIV, the science produced here has the potential to inform the global HIV response,” said Charles Gilks, from the University of Queensland. “Key to our national success has been a focus on prevention and on equitable access to care for anyone at risk of HIV.”
For Heather Ellis, a woman living with HIV and communications and engagement coordinator for Positive Women Victoria, achieving the last mile of the virtual elimination of HIV in Australia will require additional interventions – including those specifically designed to reach women.
“While the gay, bi-sexual and MSM communities are very aware of the benefit of prevention tools like PrEP, the heterosexual community is pretty much oblivious,” she said. “We need greater education – including as part of secondary school curricula – to raise awareness around how to prevent HIV, including new tools like long-acting injectable PrEP.”
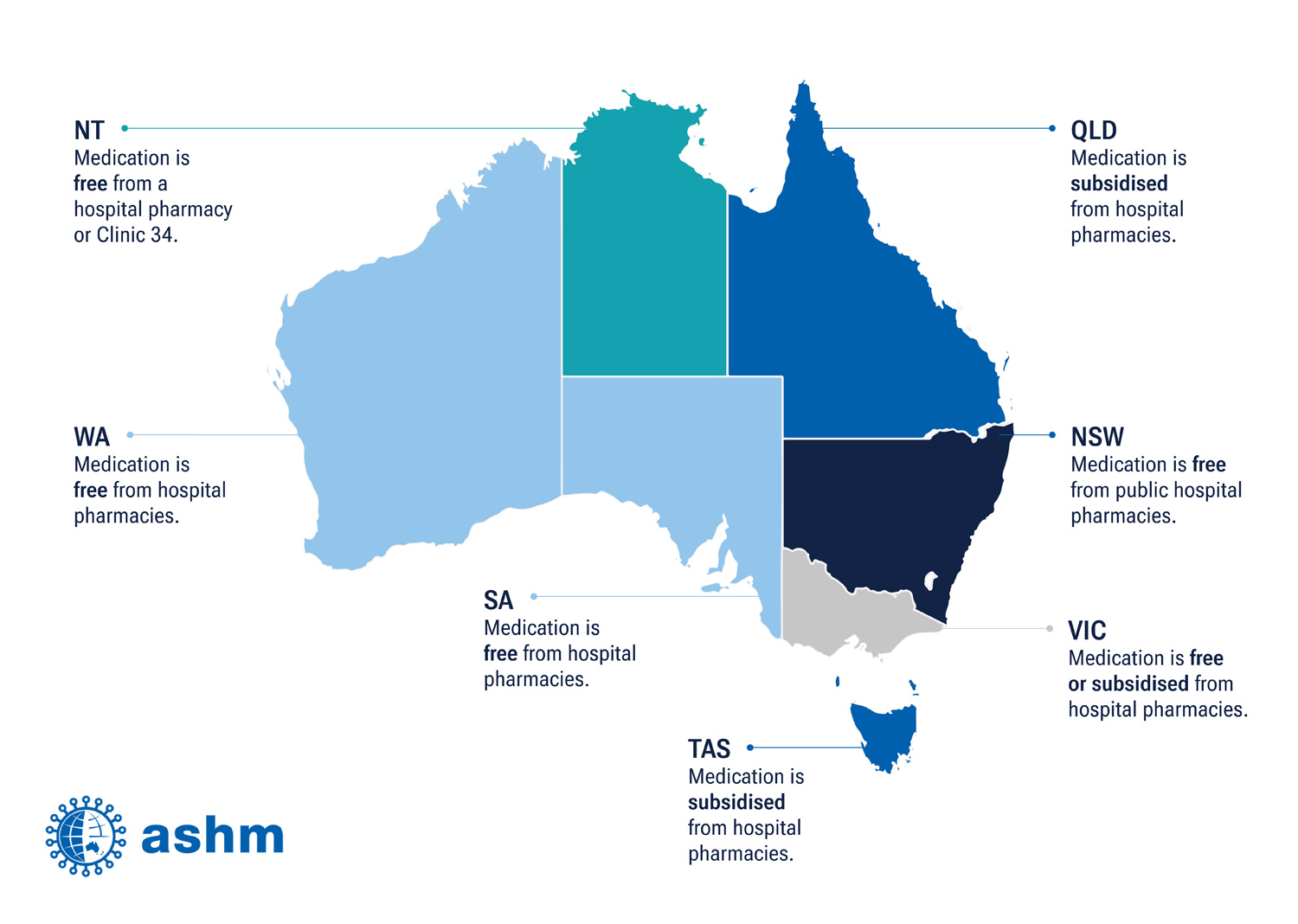 Going some way to achieve that, the government announced it was injecting $39 million for HIV treatment, which has meant that people without a Medicare card can now access government-funded HIV treatment from hospital pharmacies here in WA.
Going some way to achieve that, the government announced it was injecting $39 million for HIV treatment, which has meant that people without a Medicare card can now access government-funded HIV treatment from hospital pharmacies here in WA.
Previously, people with HIV without Medicare accessed treatment through an industry-sponsored compassionate access scheme.
To ensure medical professionals understand what these changes mean and how to provide accurate information and advice to patients, ASHM has released state-specific webinars and online resources on these new protocols at ashm.org.au.

