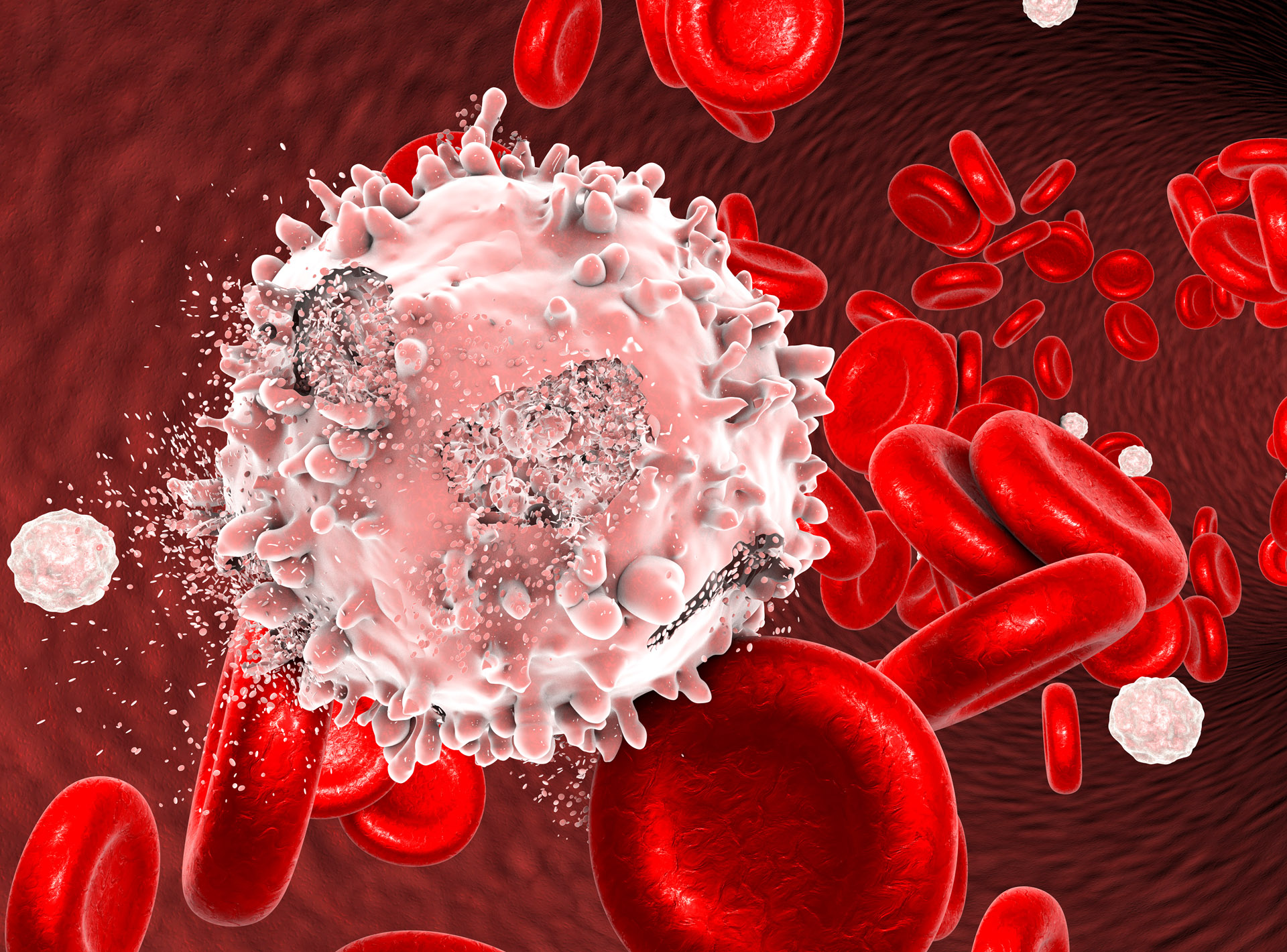
 Researchers from Australia and the US have discovered a vital new clue to improving immunotherapy to fight blood cancers such as leukaemia, myeloma, and lymphoma.
Researchers from Australia and the US have discovered a vital new clue to improving immunotherapy to fight blood cancers such as leukaemia, myeloma, and lymphoma.
The team from QIMR Berghofer and Melbourne’s Peter MacCallum Cancer Centre, found that a rare type of T cell, iNKT cells, played a critical role in improving the efficacy of a specific immunotherapy, known as ‘T cell engaging bispecific therapy’.
The iNKT cells act like a control system – alerting and guiding the body’s own T cells to attack and eliminate blood cancer cells, and by boosting their numbers, using a relatively straight forward vaccine approach to stimulate their production, the immunotherapy was significantly more effective.
The therapy has shown great potential for treating blood cancers and is already being widely tested in clinical trials. However, it had remained unclear precisely how this process worked and unlocking the science behind it was critical to further developing and improving the treatment, to ensure better long-term results.
Dr Nakamura, co-author and head of QIMR Berghofer’s Immune Targeting in Blood Cancers Laboratory, said the findings, published July 14th in the journal Blood Advances, were a big step forward in the battle against blood cancers.
“Until now, iNKT cells have been underestimated. Our research shows for the first time how important these iNKT cells are and their critical role in boosting the efficacy of the T cell engaging bispecific therapy,” Dr Nakamura said.
“Boosting the numbers of these iNKT cells has been shown to be effective and safe in patients with multiple myeloma.”
Haematologist and Director of the Centre of Excellence in Cellular Immunotherapy at the Peter MacCallum Cancer Centre, Professor Simon Harrison, explained that blood cancers are a complex group of diseases which are all linked by abnormalities in the blood cells affecting blood production and function.
“T cell engaging bispecific therapy is an off-the-shelf way that we can direct a patient’s own immune system to kill myeloma and other cancer cells, [and] we are working together to translate these findings into more effective therapies for patients,” Professor Harrison said.
According to the Leukaemia Foundation of Australia, who funded the study (with generous support from the Estate of Madella Ann Hay and the Play for a Cure Foundation), it is estimated that blood cancer is detected in 53 Australians every day and when combined, blood cancers are the second most diagnosed cancers in the country.
The Leukaemia Foundation’s CEO, Chris Tanti, welcomed the findings as another vital step towards improving health outcomes for blood cancer patients.
“We are proud to support innovative research by funding projects like this which are critical to achieving advancements in the treatment of blood cancer in this country,” Mr Tanti said.
“If we are to have any hope of reducing blood cancer mortality in Australia, we must help talented researchers to uncover powerful next generation therapies, so together we can meet our goal of zero lives lost to blood cancer by 2035.”

