ED: The burden of low back pain can respond to judicious use of non-surgical interventions by a radiologist.
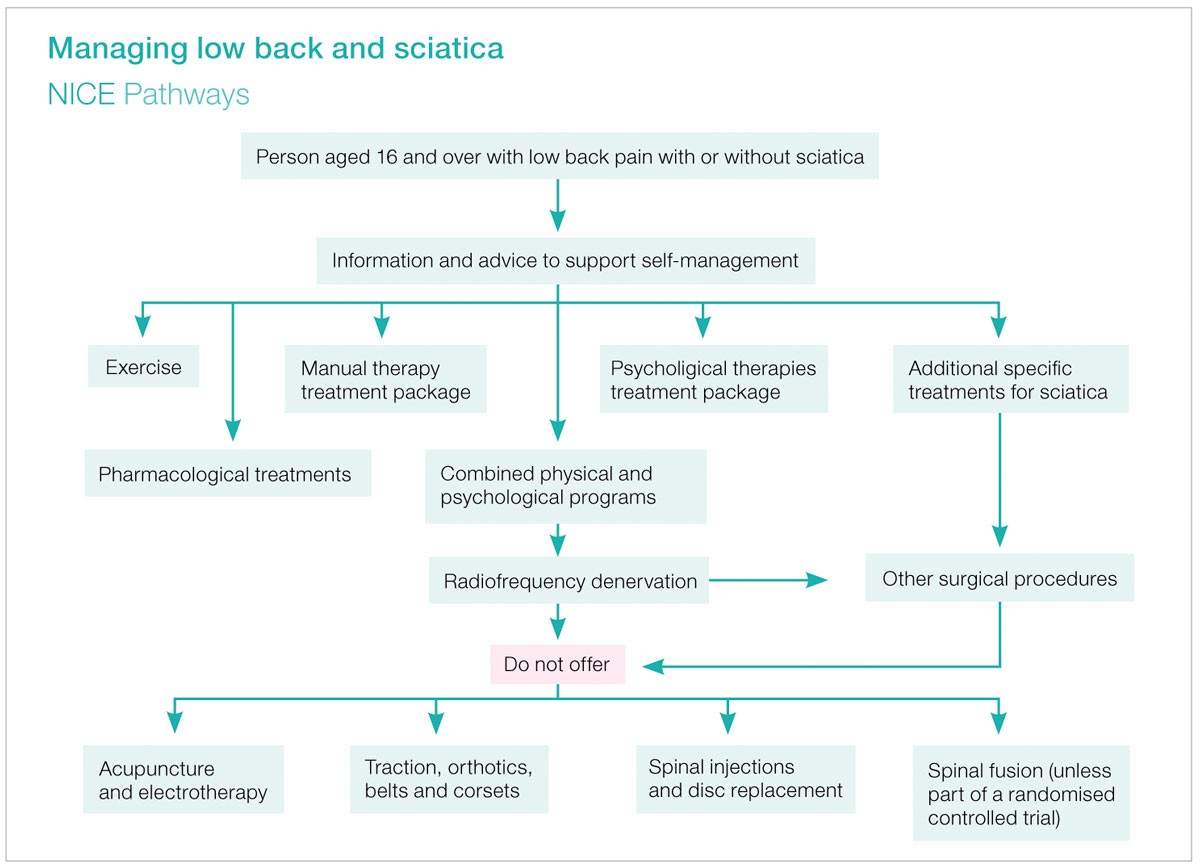
The 2017 update from the National Institute of Health and Care Excellence (NICE) recommends an algorithm (see diagram) in the treatment of low back pain +/- sciatica.
Radiologists may help diagnose and treat patients with LBP with or without sciatica (see June edition). Interventional options include facet joint injection (FJI), nerve root sleeve injection (NRSI), epidural injection, sacroiliac joint injection and radiofrequency (RF) denervation.
However, the NICE guidelines say “Do not offer” spinal injections. The authors have found FJI and NRSI to be ineffective. Nonetheless, RF denervation is a recommended treatment for LBP when there is inadequate improvement from conservative methods (e.g. physiotherapy, psychological therapy, medications and exercise).

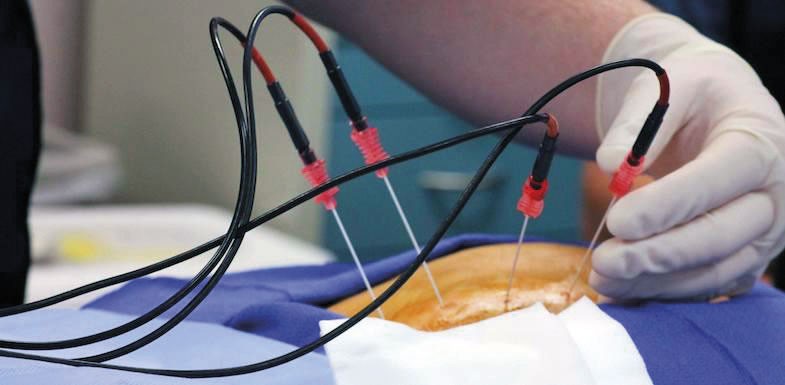
RF Denervation (or rhizotomy)
RF denervation for low back pain specifically relates to the facet joints, supplied by the medial branch of the dorsal ramus at each spinal level. Multiple facet joint levels need to be targeted as there is cross innervation of facet joints.
A trial medial branch block (MBB) or FJI is needed first to prove the facet joint is the pain source. The trial block should result in at least near-complete pain reduction with later recurrence of moderate to severe pain.
The RF procedure requires positioning of an electrode on the medial branch using CT or fluoroscopy. Nerve stimulation is confirms accurate needle localisation and then the RF electrode heats the medial branch, causing a small section of coagulative necrosis of the nerve. The lesion the procedure creates will gradually heal over time. It can be performed as an outpatient (in under 30 minutes, usually without sedation). There is frequently a period of pain flare-up (about 2 to 3 days), often followed by 12-24 months of reduced pain.
Epidural injections
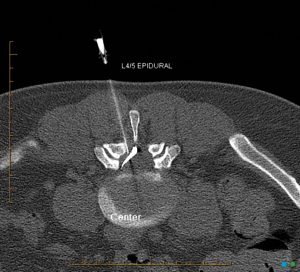
For the treatment of sciatica, the NICE guidelines suggest an epidural injection be considered if there is failure to improve with conservative management. Epidural injections are performed to treat unilateral or bilateral radicular pain. Another indication for an epidural injection is discogenic LBP, however this has not been specified in the guidelines which are only written to provide a structure to help guide management but are not all encompassing.
The procedure can use interlaminar or transforaminal (TFESI) approaches depending upon the clinical presentation and the anatomy evident on CT or MRI scan. There is likely to be a better response from TFESI and therefore you should consider requesting this method of epidural injection on a referral form.
The guidelines do not describe nerve root sleeve injections which may reduce pain in the short-term only and therefore are not considered to be cost-effective.
Spinal claudication
Central spinal canal stenosis (SCS) can present with neurogenic claudication. Similarly, some patients present with vascular claudication secondary to severe peripheral vascular disease. It is the history, physical examination, arterial Doppler and spinal imaging that differentiates the two aetiologies. The recommended treatment for spinal stenosis is decompressive surgery. There is no recommendation for epidural injection in these patients.

The pain associated with canal stenosis is due to mechanical and ischaemic factors rather than the inflammatory cascade associated with a disc herniation and radiculitis. This explains why there is only short term effect, if any, from an epidural in the setting of SCS or lateral recess stenosis.
What of anticoagulated (AC) patients?
Interventional services will have certain criteria that guide decision making in relation to AC. Cessation for some procedures can be far riskier than the risk of bleeding. It is important for the referrer to flag any AC, as well as a history of contrast allergy.
Key messages
- LBP and sciatica – try conservative management and MRI (or CT) scan only if not improving.
- If LBP due to facet joints – consider RF denervation after a positive facet joint trial block.
- Radicular pain / Sciatica – transforaminal epidural injection (TFESI) may reduce pain for short-medium term. NRSI not routinely recommended.
 References available on request.
References available on request.
Questions? Contact the editor.
Author competing interests: nil relevant disclosures.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

