By Dr Yuranga Weerakkody, Radiologist, Perth
The ultrasound-guided trans-perineal freehand prostate biopsy service was initially introduced into WA in the late 1980s by Dr James Anderson at the Royal Perth Hospital radiology department and progressively refined over the next few decades to improve patient tolerance. The service currently runs within the radiology department with clinical support and collaboration by the urology department.
Patients are initially assessed by a specialist urologist with increasing numbers of patients now also undergoing multiparametric MRI prior to biopsy. For first three decades, systematic sampling of the entire prostate was performed. With the advent of multiparametric MRI, a considerable portion of significant cancers are now discovered with targeted approaches i.e. directing the biopsies to areas in the prostate which appear suspicious on MRI.
Random systematic sampling can also be performed but tends to be performed less frequently in those with a definite MRI positive lesion with the majority of samples taken through the region of concern with a lesser number of sampling done elsewhere. The procedure can be done as an outpatient rather than a day case or main theatre, saving time and cost to the patient. There is a lower risk of sepsis and no need for routine antibiotics.

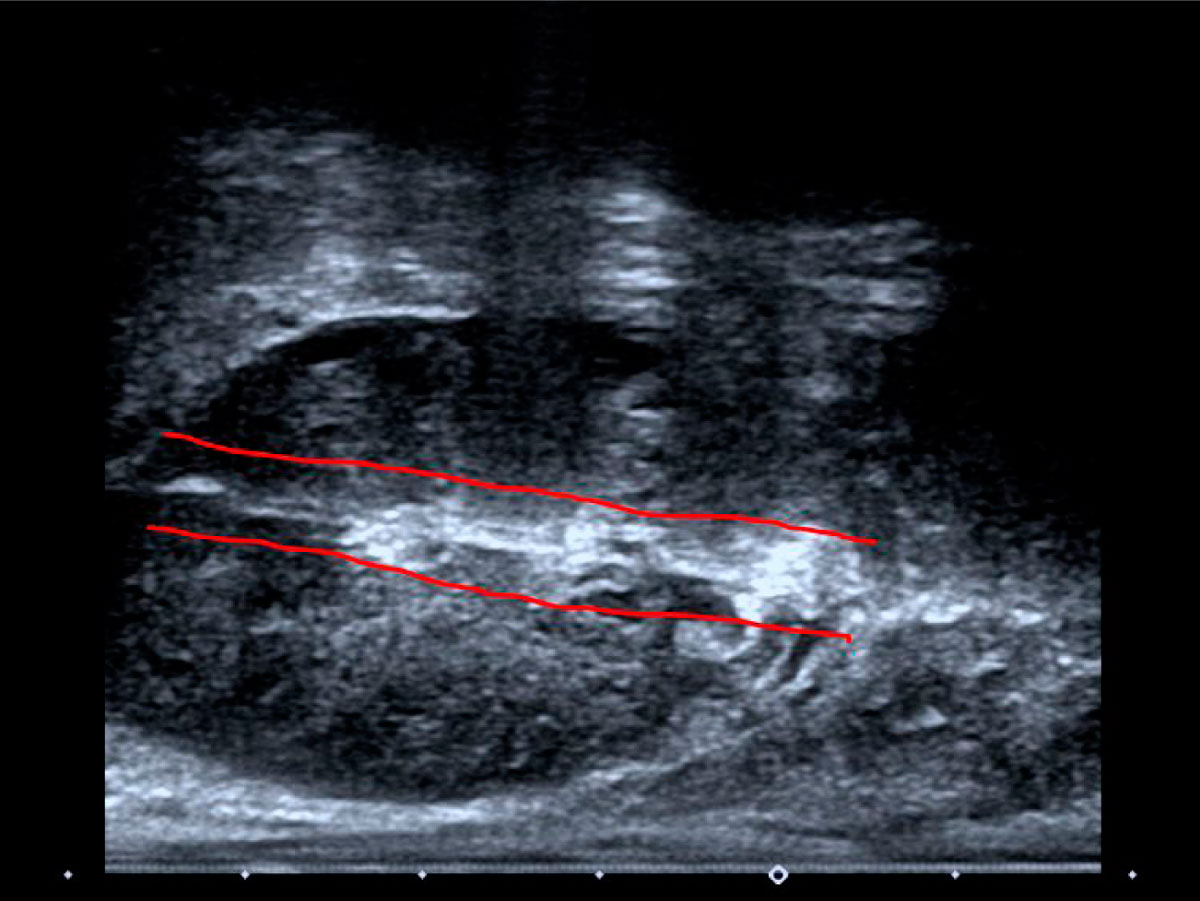
The prostate ultrasound and biopsy technique is relatively straightforward and done with the patient in the left lateral position, a bi-plane ultrasound probe is introduced into the rectum where diagnostic ultrasound images are initially taken and the prostate measured.
After obtaining consent from the patient, the perineum is cleaned with iodine. The skin, subcutaneous tissue, pelvic floor musculature and prostate capsule are then anaesthetised using local anaesthetic and under direct ultrasound guidance. Administration of local anaesthetic takes about two minutes and, after checking for numbness, the biopsies targeting the prostate are taken.
All biopsies are performed as planned procedures. Compared with a traditional trans-rectal biopsy, a trans-perineal method does require a longer period of training to acquire the sufficient skill with about 15-20 minutes procedural (on table) time and about 30-45 minutes peri-procedural time. Patients are discharged soon after but requested to remain in the hospital precinct for half an hour (usually while partaking of a beverage).
Occasionally patients do experience a vaso-vagal reaction requiring nurse supervision. Rarely, bacteremia can become manifest usually becoming clinically overt in the first 24 hours and patients are instructed to contact the referring urologist and or general practitioner if they experience symptoms.
The author acknowledges the input of Drs James Anderson, Mikhail Lozinskiy and Tanya Ha
Key messages
- Ultrasound-directed transperineal prostate biopsy can be an outpatient procedure
- MRI can guide to biopsy site(s)
- Sepsis is considered less than that with trans-rectal biopsy
References available on request.
Questions? Contact the editor.
Author competing interests: nil
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

