The Peter Doherty Institute for Infection and Immunity and researchers from UNSW Sydney have found that while immune cells in older adults resemble those in newborns and children, they have clocked out when it comes to virus detection.
The world-first discovery revealed that T cells in older adults, directed against influenza viruses, closely resemble those found in newborns and children, but struggle to recognise infected cells – a finding that unlocks the potential for the development of better vaccines and therapies tailored to different age groups.
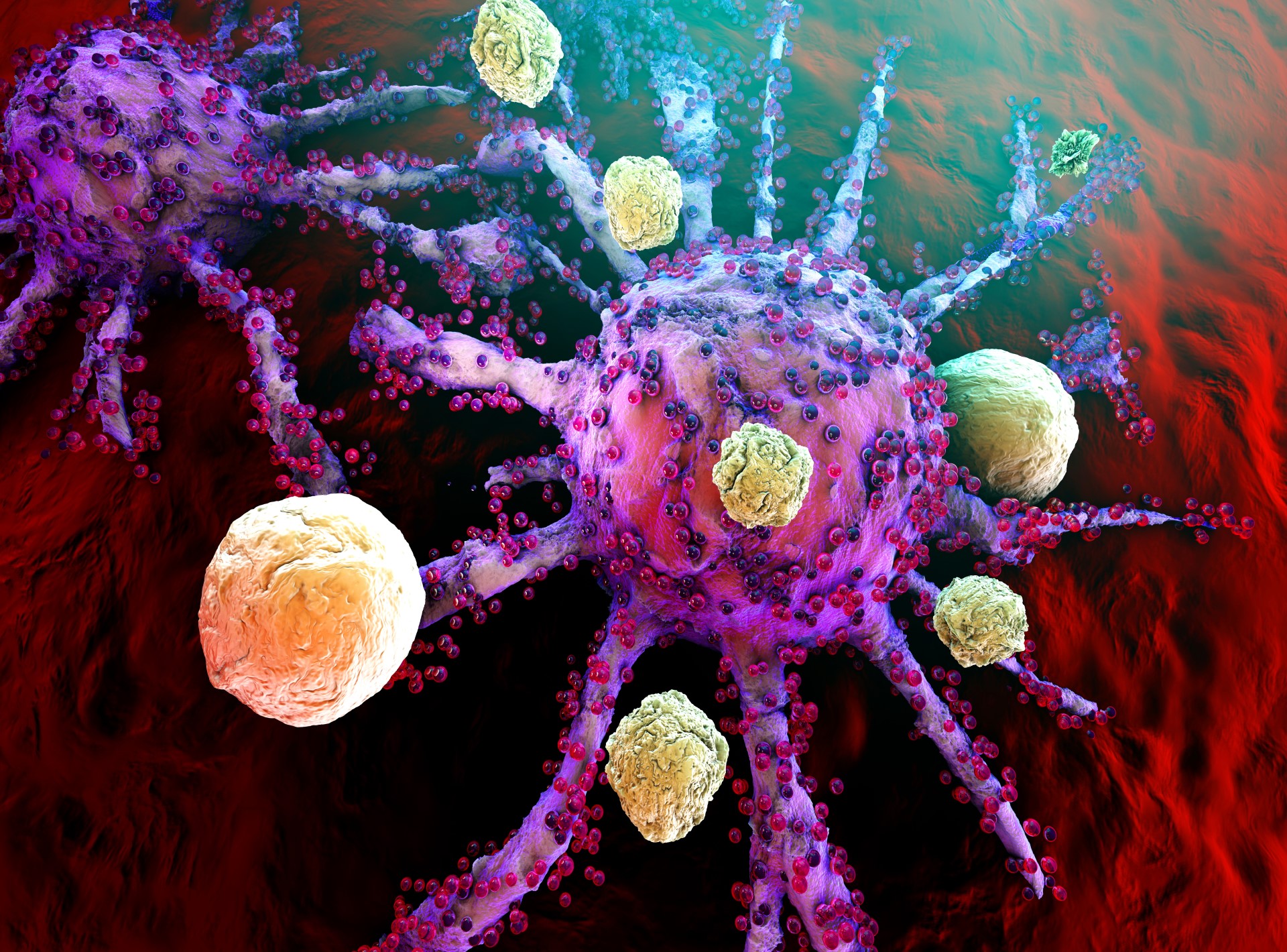
CD8+ T cells play a critical role in the immune system by eliminating virus-infected cells. While much has been studied about these immune cells in adults, little was known about how they evolve and function across the human lifespan – until now.
The study, published in Nature Immunology, employed innovative technologies to examine killer T cells in different age groups – newborns, school-aged children, adults, and older adults (60+ years) – to understand how age shapes our immunity to influenza viruses.
University of Melbourne’s Dr Carolien van de Sandt, a Senior Research Fellow at the Doherty Institute and lead author, said the team uncovered unexpected similarities in T cell responses between newborns/children and older adults.
“Based on previous studies, we expected to find that killer T cells in older adults were less effective because they had become exhausted or ‘fallen asleep,’” Dr van de Sandt said.
“However, to our surprise, the very efficient CD8+ cells that we detected in children and adults seemed to disappear and be replaced with suboptimal cells in older adults. It is almost as if you replace the sword of a Roman soldier with a kitchen knife; they can learn how to use it, but it will never be as efficient as the sword.
“One of the most intriguing findings of the study was that these cells, with a lower ability to recognise influenza viruses, displayed gene features closely similar to T cells found in newborns.”
The team specifically examined CD8+ T cell immunity directed at the prominent influenza epitope HLA-A*02:01-M158–66 (A2/M158) across four age groups at phenotypic, transcriptomic, clonal, and functional levels.
For the ‘lifespan’ cohort, they recruited healthy HLA-A*02:01-expressing individuals across four immunologically distinct age groups: newborns (n = 11, 0 years), children (n = 12; median 9 years, range 3–16), adults (n = 20; median 37 years, range 18–58) and older adults (n = 18; median 72 years, range 63–88).
“We identified a linear differentiation trajectory from newborns to children then adults, followed by divergence and a clonal reset in older adults. Gene profiles in older adults closely resemble those of newborns and children, despite being clonally distinct,” the authors explained in the study.
“Only child-derived and adult-derived A2/M158+CD8+ T cells had the potential to differentiate into highly cytotoxic epitope-specific CD8+ T cells, which was linked to highly functional public T cell receptor (TCR)αβ signatures.”
The public TCRαβ clonotype was first identified in children, peaked in adults, and decreased in older adults, coinciding with large private TCRαβ expansions and during infections, ‘best-fit’ high-avidity clonotypes are selected from naive TCR repertoires and expand following subsequent encounters.
“Unexpectedly, older A2/M158+CD8+ T cells did not reach terminally differentiated or exhausted end points. Instead, reduced functionality was associated with loss of highly functional public TCRαβ clonotypes dominating younger TCRαβ repertoires,” Associate Professor Fabio Luciani from UNSW Sydney explained.
“As individuals grow, killer T cells get stronger and more effective at eliminating infected cells, but they disappear in older adults, where they are taken over by cells with a lower killing capacity. Suboptimal TCRαβ signatures in older adults led to less proliferation, polyfunctionality, avidity and recognition of peptide mutants, although they displayed no signs of exhaustion.”
University of Melbourne’s Professor Katherine Kedzierska, Head of the Human T cell Laboratory at the Doherty Institute and a senior author, said the research was a turning point for research into ageing immunity.
“This data suggests that priming T cells at different stages of life might greatly affect CD8+ T cell responses toward viral infections,” she said.
“Knowing that timing may play an essential role in maintaining these optimal T cells into old age, has far-reaching implications and opens new possibilities for the development of better vaccines and therapies tailored to different age groups.
“We demonstrated that ‘best-fit’ high-avidity public clonotypes peak in adults and are gradually replaced by low-avidity clonotypes in older adults, and understanding how we can preserve this delicate balance, between expansion of ‘best-fit’ TCRs while maintaining TCR diversity, may be the Holy Grail in defining how we can maintain optimal immunity across the human lifespan through vaccination and/or immunotherapies.”