This content is part of a paid partnership with The Vein Clinic.
Disrupted normal anatomy and negative patient psychology (“what’s the point treating, they will just come back”) present significant challenges to the physician treating recurrent varicose veins (RVV).
Dr Matar is a dual-qualified Radiologist and Phlebologist. His personal and family history with varicose veins fuels his ongoing passion for offering the most effective varicose vein treatments available.
As medical director of The Vein Clinic in Perth he has pioneered several innovations in vein treatment and offers a highly tailored and targeted approach to treating venous insufficiency, the cause of varicose veins and a frequent cause of restless legs.
The literature and our own experience highlight three common and largely preventable causes of RVV:
- Diagnostic error – incomplete identification of all reflux points
- Treatment error – inadequate treatment of all reflux points
- Lack of follow-up and ongoing maintenance.
Ultrasound diagnosis
The standard of care before any vein intervention should be a detailed doppler study of the deep and superficial venous system.
Whilst nearly all general sonographers are competent at DVT studies, a smaller subset of vascular sonographers are fully competent at specialised chronic venous insufficiency (CVI) studies.
Typically, non GSV/SSV causes of reflux, including accessory veins, pathological perforator veins, pelvic veins and anomalous veins may not be properly assessed. Deep vein reflux and obstruction may also go unrecognised leading to RVV.
Incomplete or inappropriate treatment
Incomplete diagnosis will of course lead to inadequate treatment. Historically, phlebectomy without treating underlying saphenous reflux, not surprisingly, resulted in high rates of RVV.
High ligation and stripping (HLS) is still practised despite strip-track revascularisation and groin neovascularisation in up to 80% of patients on ultrasound studies; albeit with a much lower rate of clinical recurrence.
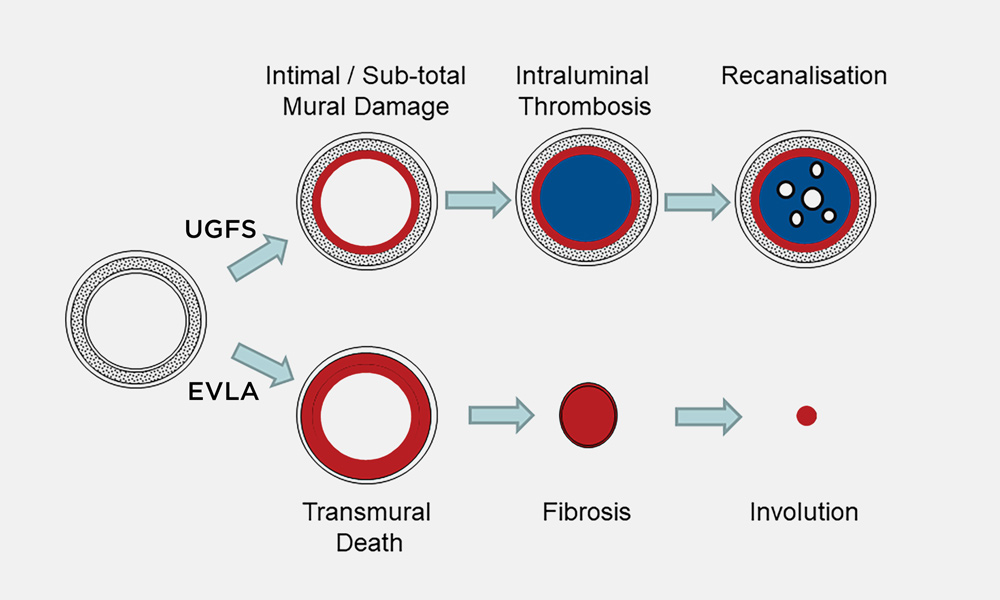 Ultrasound Guided Foam Sclerotherapy (UGFS) has been shown to have only an overall success rate of around 50%. Whilst a useful adjunct procedure, particularly for smaller veins, the science, literature, and our own experience supports that this is rarely a satisfactory standalone treatment for refluxing saphenous veins.
Ultrasound Guided Foam Sclerotherapy (UGFS) has been shown to have only an overall success rate of around 50%. Whilst a useful adjunct procedure, particularly for smaller veins, the science, literature, and our own experience supports that this is rarely a satisfactory standalone treatment for refluxing saphenous veins.
The success of UGFS depends largely on the size and wall thickness of the vein being treated, but is also highly influenced by the choice and concentration of sclerosant as well as the method of administration and skill/experience of the operator.
Endothelial damage from sclerosant action in larger veins will often result in temporary closure from “sclerothrombus”, with subsequent clot and fibrinolysis resulting in recannalisation and recurrent reflux leading to RVV.
Endothermal ablation methods (EVLA/RfA) are now clearly established internationally as the gold standard for treating incompetent saphenous veins. Success is far less operator-dependent than with UGFS, closure rates >95% are commonly seen across all operators.
Endothermal ablation failures may occur when the wrong veins are treated, inadequate energy is used to close the veins, and incomplete treatment of reflux has occurred (i.e., accessory veins, perforator veins and lowest reflux point not treated) problems that are commonly seen with novice operators.
The diagram (below left), reproduced with permission from Professor Mark Whiteley, illustrates the subtotal vein damage and subsequent recannalisation common following UGFS compared to full-thickness wall damage and true vein involution usual following EVLA.
Incomplete/non-existent follow-up
Further research from The Whiteley Clinic has shown that varicose veins may still develop at a de novo rate of around 3% per year despite optimal treatment technique.
If optimal treatment has been performed, new varicose veins will normally develop in veins that were previously disease-free. This represents natural disease progression and not treatment failure.
It is for this reason that many dedicated vein clinics recommend annual sonographic surveillance and clinical follow-up so that RVV are detected and treated early, when they are less extensive and expensive to treat.
Questions? Contact the editor.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website

