This content is part of a paid partnership with Clinipath Pathology. 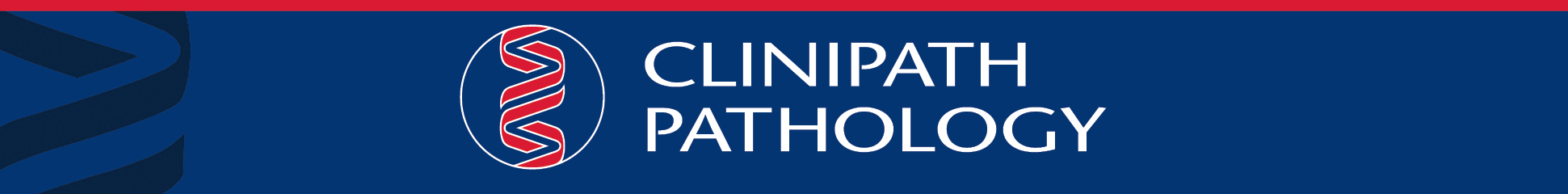
Differentiation of intestinal tuberculosis from Crohn’s disease can be challenging due to overlapping clinical, endoscopic and histopathologic features. However, this distinction is important as treatment for these two conditions differs considerably.
We present a case where clinical and pathological suspicion were important factors in reaching a diagnosis, despite absence of acid-fast bacilli in tissue sections and negative microbiological molecular testing.

Case history
A 27-year-old female, originally from Bhutan with a history of latent tuberculosis, underwent upper and lower gastrointestinal endoscopy to investigate a history of abdominal pain and iron deficiency.
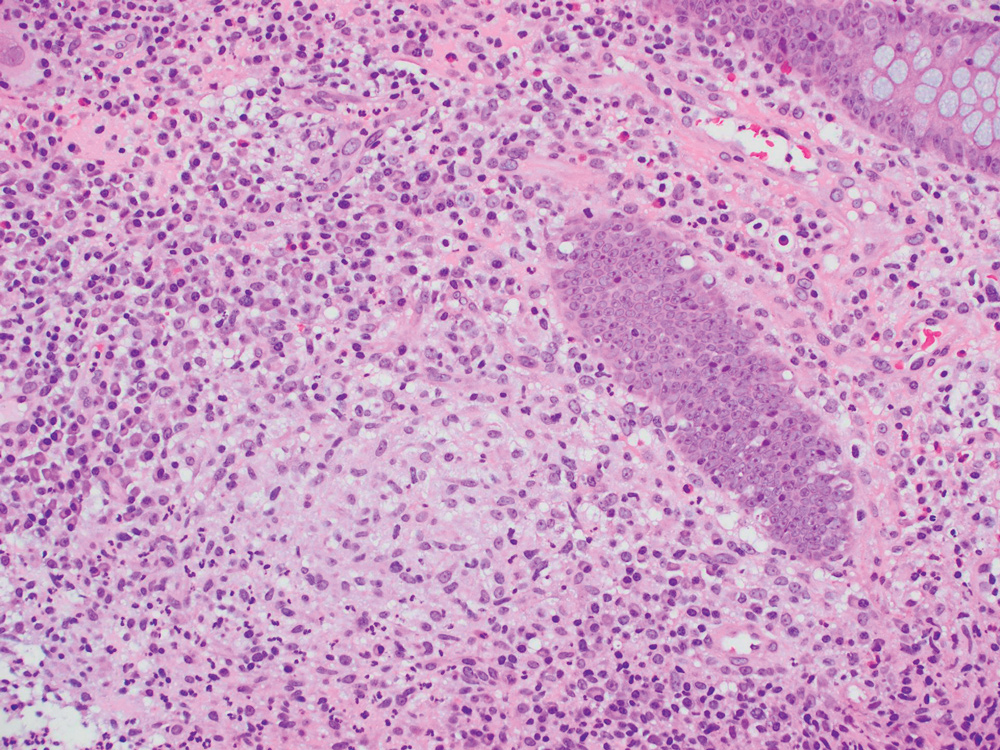
Upper GI endoscopy was normal. However, colonoscopy demonstrated a segmental ileocolitis involving the ileum, caecum, ascending colon and transverse colon, with features of chronicity. The clinical features were suggestive of Crohn’s disease although given the patient‘s history, mycobacterial colitis was in the differential diagnosis.
Histopathological examination showed active ileo-colitis with ulceration, non-necrotising granulomatous inflammation and only subtle architectural distortion. Mycobacterial and fungal organisms were not detected with special stains.
Although Crohn’s disease was a consideration, there were no well-developed features of chronicity. In spite of the absence of acid-fast bacilli on special stains, the microscopic findings were concerning for mycobacterial infection.
TB PCR testing performed on the formalin fixed biopsy tissue was negative.
A repeat colonoscopy was performed to obtain fresh tissue and the culture of this fresh colon biopsy tissue subsequently grew mycobacterium tuberculosis.
Discussion
TB-associated granulomatous colitis can mimic Crohn’s disease clinically and in the absence of other clinical manifestations of TB, differentiating between intestinal TB and Crohn’s disease can pose a significant diagnostic challenge.
Both diseases can present with clinical symptoms of weight loss, abdominal pain, fever, bowel obstruction, bloody diarrhoea and endoscopic findings of skip lesions, ulcerations and terminal ileum involvement. Diagnostic histopathologic features of intestinal TB such as confluent caseating granulomas within the submucosa and acid-fast bacilli are infrequently seen in biopsies and these features were not present in this case.
The diagnosis of intestinal TB and Crohn’s disease requires a high degree of suspicion, especially when encountering a patient originally from an endemic area.
Special stains such as Ziehl -Neelsen (ZN) and PCR-based assays are used for rapid detection of mycobacterial infection; PCR-based tests have high sensitivity and specificity although cannot differentiate between viable and non-viable organisms.
They may remain positive for prolonged periods after the patient has been treated with anti-TB therapy and therefore are of limited use in follow-up of known TB cases.
In addition, PCR assays may have limited sensitivity in detecting extrapulmonary mycobacterial infections. A negative ZN stain or tissue PCR therefore does not exclude a diagnosis of TB and mycobacterial culture remains the gold standard for definitive diagnosis. It is therefore important that in cases where the index of suspicion for intestinal TB is high, fresh biopsy material should be obtained for culture.
– References on request
Questions? Contact the editor.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website

