
Heart disease is a leading cause of death in people with diabetes mellitus. Despite improvements in treatment options, diabetes remains associated with excess risk of heart disease. This is particularly important in people with diabetes with recent heart attack as the risk of recurrent heart attack, heart failure and death are increased substantially.
Previous studies have consistently demonstrated strong associations between high blood sugar in the immediate aftermath of heart attack and increased risk of recurrent heart attack, heart failure or death. Furthermore, studies in heart attack settings have shown that high blood sugar during inpatient admission is frequently overlooked and inadequately addressed.
Recent large-scale studies suggest that a new class of diabetes medications, sodium-glucose cotransporter-2 inhibitors (SGLT2Is), improve outcomes in patients with type 2 diabetes and heart diseases especially the high risk patients such as those with heart failure. Indeed, in patients with type 2 diabetes and heart failure, SGLT2Is are being increasingly prescribed by specialists and family doctors.
The question that is often asked is can they be started early following heart attack in patients with diabetes?
Despite the well-established benefits in heart disease patients especially those with heart failure, studies have shown that the perceived side effect concerns have precluded their widespread use especially when patients are still in the hospital following the heart attack. This is troublesome, as it is known that initiation of treatment prior to hospital discharge improve medication adherence and long-term outcomes.
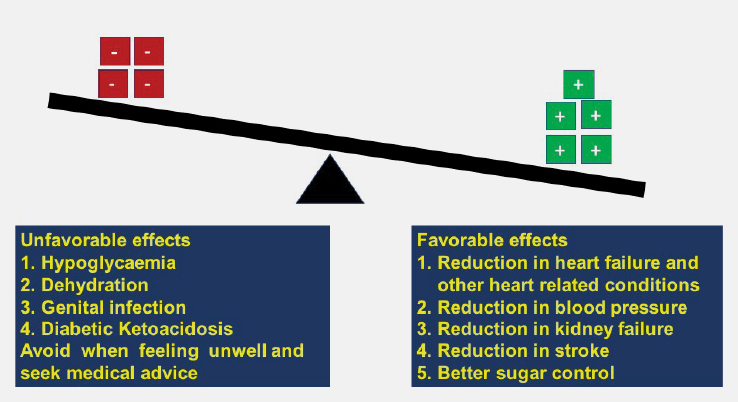
Preliminary small studies have shown that SGLT2Is can be safely started in a majority of patients following a heart attack. Early treatment would improve medication compliance and also reduce chances of complications such as heart failure, stroke, kidney failure and death in these patients. Ongoing studies, including the study funded by Diabetes Research WA and being performed at the Fiona Stanley Hospital, will provide further evidence of the safety and usefulness of this drug in heart attack patients especially when started soon after the heart attack.
Other pertinent questions are what are the possible side effects of SGLT2Is and should one temporarily stop taking this medication when feeling unwell?
Uncommon but possible side effects of SGLT2Is include hypoglycaemia (low blood glucose – this usually only occurs if SGLT2 inhibitors are used in combination with other diabetes medicines), dehydration, an increased risk of infection such as thrush around the genitals and rarely observed effect of an increase of acid in the blood (diabetic ketoacidosis). If a patient has been told about an active foot ulcer or circulatory problem in a leg, they should discuss with a doctor before continuing this medication. If the patient is feeling unwell (vomiting, diarrhoea, fever, sweats and shaking), they should also temporarily stop taking this medication and seek medical advice.
Key messages
- Diabetes remains a significant risk factor for heart disease
- Research shows that use of SGLT2Is can improve outcomes
- Early treatment can be undertaken safely in stable patients.
Author competing interests – the author is involved in research mentioned in the article

