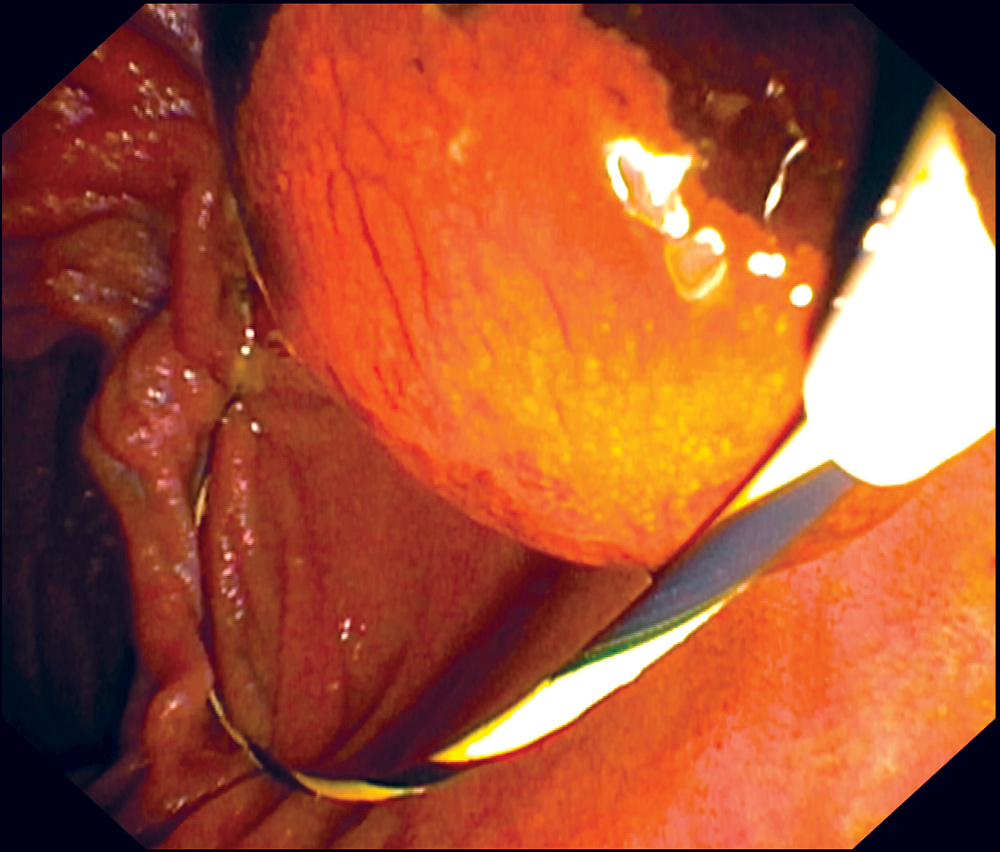
Endoscopic retrograde cholangiopancreatography (ERCP) has evolved from a diagnostic tool to an almost exclusively therapeutic procedure. ERCP is performed with a side-viewing duodenoscope that allows identification of the major papilla. The bile duct is cannulated under endoscopic and fluoroscopic guidance (image 1) and a variety of catheters, balloons, baskets, guidewires, and stents are used for therapeutic interventions (image 2).

Indications
Patients with any of the urgent indications should be referred to nearest Emergency Department, after contacting the ERCP fellow or on-call gastro registrar.
Acute cholangitis: characterised by fever, jaundice and abdominal pain and is a medical emergency with high mortality if not treated promptly. ERCP should be performed within 48 hours (preferably < 24 hours).
Acute pancreatitis with concomitant cholangitis: ERCP should be performed within 24 hours of presentation with gallstone pancreatitis and cholangitis.
Obstructive jaundice due to CBD stone or malignancy: (pancreatic carcinoma, cholangiocarcinoma or ampullary adenocarcinoma).
Patients with malignancy are discussed in a multidisciplinary team meeting with Hepato-pancreato-biliary surgeons and depending on the clinical presentation, some of these patients undergo ERCP for biliary drainage.

Patients with non-urgent indications should be referred to a tertiary hospital or a private interventional gastroenterologist for an ERCP in following conditions:
- Symptomatic choledocholithiasis
- Retained biliary stones post cholecystectomy
- Bile leak post cholecystectomy (generally, these patients are reviewed and referred by the treating surgeon)
- Benign biliary strictures
- Sphincter of Oddi dysfunction (type 1) – biliary-type pain, abnormal LFTs, and dilated common bile duct.
Contraindications
ERCP is primarily a therapeutic procedure and should be avoided in the following situations:
- Diagnostic test for abdominal pain without evidence of biliary obstruction.
- Biliary-type pain with normal LFTs and non-dilated CBD (type III SOD).
- Biliary-type pain and either abnormal liver tests or a dilated common bile duct – some of these patients may considered for ERCP after review by a gastroenterologist.
- Patient with surgically altered anatomy (e.g., Roux-en-Y anatomy). ERCP can be performed in patient with altered anatomy with a surgically created stoma or access.
- Diagnostic test for pancreatic cysts/pancreatography.
Complications
Despite the technical advances, appropriate patient selection, focus on adherence of safety protocols and advanced training programs, ERCP remains a procedure with high complication rates as compared to any other endoscopic procedures.
The incidence of post ERCP pancreatitis (PEP) ranges from 3-5%. Severe pancreatitis (pancreatitis with persistent organ failure lasting over 48 hours) is reported in 0.1-0.7%. Administration of per rectal indomethacin or diclofenac and insertion of pancreatic duct stent (in cases of inadvertent pancreatic duct cannulation) at the time of procedure, has shown to decrease rates of PEP.
Post sphincterotomy bleeding is more common during procedure or in first 24 hours, however, it can occur up to seven days post procedure. Risk of bleeding is 1-3% and the risk of clinically significant bleeding requiring extended hospital admission or endoscopic management is 0.2%.
Incidence of post ERCP cholangitis is 0.5-3% (most often due to incomplete drainage of obstructed or infected biliary tree). Other less common complications are post ERCP cholecystitis, perforation, bacterial peritonitis in patients with cirrhosis and anaesthetic-related complications.
Aside urgent indications, most ERCPs are done as a day case and post-ERCP complications happen after discharge with patients presenting to their GPs. Below are a few things to consider while managing post-ERCP patients in the community:
- Early referral to ED in case of bleeding (haematemesis, melaena, dizziness or palpitations), cholangitis (fever, abdominal pain and jaundice) or pancreatitis.
- Removal or replacement of stents: The team performing ERCP is responsible for organising follow-up procedures for patients with pancreatic duct or biliary stents. However, to ensure that patients are not lost to follow-up, it is important for GPs to be aware of:
- Pancreatic duct stent: An abdominal X-ray should be requested by the GP, 7-10 days post-procedure in cases where a pancreatic duct stent was placed during ERCP, and if the stent is still in-situ, inform the treating gastroenterology team to organise another ERCP or gastroscopy for its removal.
- Biliary stent: ERCP reports should mention the indication of plastic biliary stent (e.g., incomplete biliary clearance or CBD stricture) and the plan for its removal or replacement. GPs should contact the treating gastroenterology team if the indication of stenting is not mentioned in the report and a repeat procedure is not performed in a timely manner.
Key messages
- ERCP is primarily a therapeutic procedure
- Diagnostic ERCP is rarely performed nowadays, and unnecessary procedures should be avoided.
- Early recognition and prompt referral of post-ERCP complications is critical as most procedures are day cases and complications can develop up to seven days later.
Author competing interests – nil

