Atrial fibrillation (AF) is one of the commonest causes of stroke (particularly debilitating stroke). Thromboembolism usually occurs when thrombus is dislodged from the left atrial appendage (LAA). It is estimated that 90% of emboli in patients with AF come from the left atrial appendage.

Embolism may occur to the brain with silent or clinically overt, often debilitating, stroke. Clots may embolise to other organ systems with or without overt sequelae (e.g., acute gut ischemia, acute upper or lower limb ischemia, myocardial infarction).
Anticoagulation is a standard treatment in most patients with AF to prevent thromboembolism and stroke. The annual risk of stroke is lowered by approximately two thirds by anticoagulation, with those patients at highest risk of embolic stroke (high CHA2DS2-VASc score) accruing the most absolute benefit.
Because anticoagulation is associated with an increased risk of bleeding the prescription of an anticoagulant involves careful discussion with the patient about relative risks and benefits. The HAS-BLED score is perhaps the most accurate of a number of bleeding risk scores. However, all are relatively imprecise, especially for the individual patient. An anticoagulant is relatively or absolutely contraindicated in some patients.
While stroke prevention is the major imperative in high-risk patients with AF, other treatment strategies are considered concurrently. Rate control in patients with AF provides symptomatic relief and, in some patients, restoration of sinus rhythm (SR) rhythm control is appropriate.
Rhythm control can be achieved by management of co-morbid conditions (weight reduction, reduction of alcohol intake, treatment of sleep apnoea, hypertension control, physical activity). Other rhythm control strategies include pharmacologic therapies, percutaneous catheter ablation of atrial fibrillation and/or a variety of surgical procedures which have been developed to diminish the burden of AF.
Successful rhythm control (restoration of sinus rhythm) has not been proven to abolish the risk of thromboembolism, and this is particularly so in patients with a high risk of thromboembolism and stroke. Most patient with AF who have a catheter or surgical ablation procedure, or in whom a pharmacologic strategy is used require ongoing anticoagulation.

Indications for LAAO
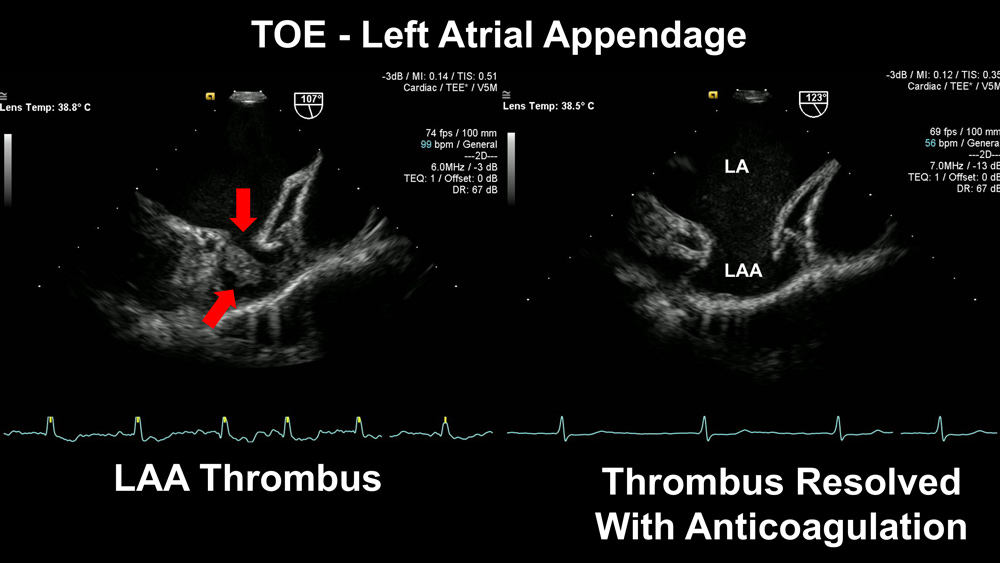
Oral anticoagulation remains the standard of care for patients with atrial fibrillation and significant risk of thromboembolism, assuming there is no relative or absolute contraindication to prescription of an anticoagulant drug. Thrombus in the left atrial appendage can resolve after even short periods of anticoagulation. (Fig.1)
Occlusion of the LAA is an alternative strategy to reduce the risk of thromboembolism and stroke when anticoagulants are relatively or absolutely contraindicated. There is currently no proven role for percutaneous LAAO in patients without AF. In patients with AF who have an embolic event while anticoagulated, LAAO can be considered as an adjunctive therapy, but this treatment has not been scientifically proven.
In percutaneous occlusion (LAAO) the left atrial appendage may be occluded percutaneously under local or general anaesthesia using one of a number of approved devices ( Fig. 2, closure of atrial appendage using Amplatzer Amulet Device). Analysing the data available to date indicates that percutaneous LAAO provides a similar reduction in stroke risk compared with standard oral anticoagulation.
Surgical LAAO
Historically, the left atrial appendage has sometimes been occluded at the time of open-heart surgery. Amputation and closure using a stapling device, and linear closure from within the left atrium are well established surgical techniques. More recently, stand-alone thoracoscopic LAAO is performed in a procedure which is relatively quick, minimally invasive, and effective.
In patients with AF where anticoagulation is appropriate but there is a significant relative or absolute contraindication to anticoagulants, LAAO should be considered. Those patients at highest risk of stroke are likely to accrue the most benefit.
While the various strategies to provide rate and rhythm control in AF are important it is crucial to be cognisant that a successful catheter or surgical ablation procedure, or pharmacologic reduction of AF burden has not been proven to correlate directly with a reduction in thromboembolic risk, particularly in patients at high risk of stroke.
It is essential that there is a careful discussion with high-risk AF patients about thromboembolic risk, and when anticoagulants are contraindicated that LAAO should be discussed.
Key messages
- Thromboembolism from the left atrial appendage in patients with AF is a major cause of stroke
- Pharmacologic rhythm control, catheter or surgical ablation procedures may reduce the burden of AF but have not been proven to eliminate the thromboembolic risk, particularly in high-risk AF patients
- Closure of the LAA by percutaneous or stand-alone surgical techniques should be considered in all patients with AF in whom anticoagulants are contraindicated.
The author acknowledges Dr Phillip Currie for the images.
– References available on request
Author competing interests – nil

