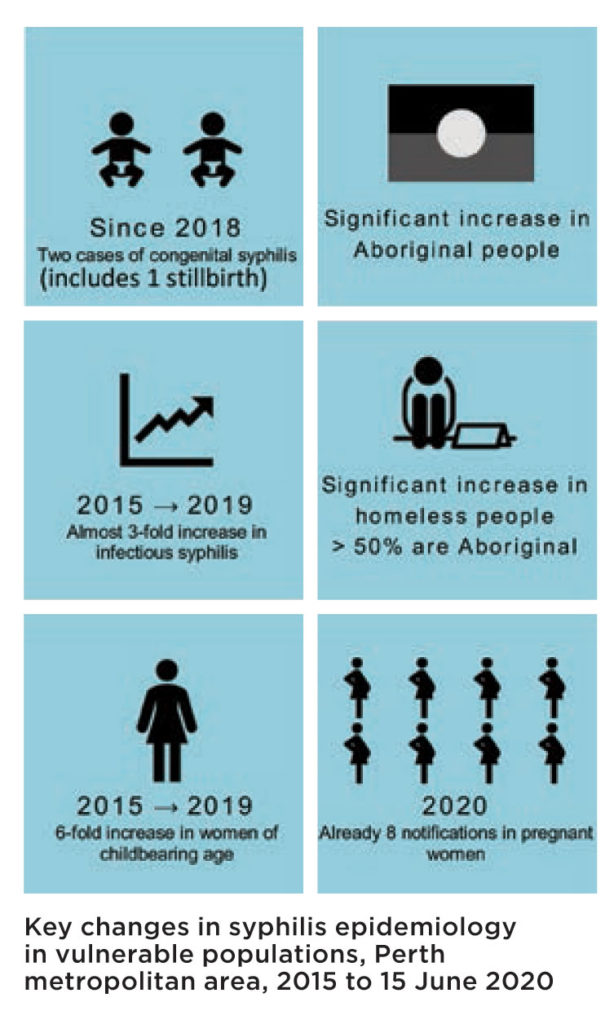
Over the past decade syphilis in the Perth metropolitan area has occurred primarily amongst men who have sex with men (MSM).
However, there is increasing diversity in those affected, with a pronounced increase in cases among vulnerable groups, including Aboriginal people, women of childbearing age, people who inject drugs and homeless people.

Between 2015 and 2019 there has been a threefold increase in infectious syphilis notifications in the metropolitan area. In the past 18 months there have been 26 notifications among homeless people, compared to six in the previous four years.
There have been 57 notifications in Aboriginal people in the past 18 months, compared to 23 notifications in the previous four years. In the first half of 2020 there have been eight notifications in women who were pregnant at the time of diagnosis. Most alarmingly, there have been two cases of congenital syphilis in Perth since 2018, including a stillborn, preterm child delivered in a hospital emergency department.
In response to the changing epidemiology, the WA Department of Health’s Chief Health Officer has declared a syphilis outbreak in vulnerable groups in the Perth area, affecting:
- People experiencing homelessness, including couch surfing
- People experiencing acute mental illness
- People who inject drugs
- Young Aboriginal and non-Aboriginal people
- Culturally and linguistically diverse people
Clinicians should offer screening for syphilis in all persons attending for diagnosis and treatment of any STI, or where screening for STIs is indicated. This is particularly important among pregnant women and women of child bearing age.
Be aware that most pregnant women are sexually active and some change sex partners during pregnancy. Offer opportunistic syphilis blood testing to patients from the identified vulnerable populations whenever they present for healthcare, including, antenatal, drug treatment and primary health care services.
Whilst engaging in conversations and risk assessment regarding sexuality and sexual behaviours can be complex and may take some clinicians and their patients outside of their comfort zones, it is important to be having these conversations to raise awareness of the increasing risk of syphilis.
When talking about risk of STIs, remember to:
- Emphasise that the purpose of the conversation is to detect and treat STIs early to minimise the risk of transmission and long-term health issues caused by undiagnosed disease, including syphilis;
- Use gender neutral pronouns for partners;
- Reassure the patient about confidentiality;
- Not to assume anything about the patient’s sexual behaviours or those of their sexual partner/s;
- Ask about other risk factors for STIs and blood-borne viruses such as injecting drug use, including methamphetamine.
Infectious syphilis should be treated with benzathine penicillin 2.4 million units IMI stat, given as a half dose into each buttock using pre-filled syringes. Benzathine penicillin is available free via the PBS doctor’s bag. It is important to take a blood test for syphilis on the day of treatment so the response to treatment can be monitored. Contacts of a confirmed syphilis case should receive the same treatment empirically, at the time of testing.
 All newly diagnosed cases of syphilis should be notified promptly to the Department of Health. Doctors may also contact Metropolitan Communicable Disease Control (MCDC) on 9222 8588, Mon-Fri 8am-5pm for assistance with contact tracing and advice on management.
All newly diagnosed cases of syphilis should be notified promptly to the Department of Health. Doctors may also contact Metropolitan Communicable Disease Control (MCDC) on 9222 8588, Mon-Fri 8am-5pm for assistance with contact tracing and advice on management.
To support both the community and the health sector to increase education and awareness on the diagnosis and treatment of syphilis, a suite of resources is available through dohquickmail.com.au. The WA Department of Health has also commissioned a professional development online learning platform that can be accessed free of charge at lms.ashm.org.au. Resources and guidelines are also available at https://ww2.health.wa.gov.au/Articles/U_Z/WA-Syphilis-outbreak-response.
Further information regarding STI testing, management and contact tracing is available at http://ww2.health.wa.gov.au/Silver-book – WA Guidelines for Managing Sexually Transmitted Infections (Silver Book).
Key changes in syphilis epidemiology in vulnerable populations, Perth metropolitan area, 2015 to 15 June 2020

