 A sexually active 30-year-old woman presents with a rash and wrist pain, among other symptoms.
A sexually active 30-year-old woman presents with a rash and wrist pain, among other symptoms.
Background
A 30-year-old woman presents with a 1-week history of severe right upper quadrant abdominal pain, bilateral shoulder and wrist pain, fever, and chills. She also has a rash, which developed 2 weeks ago and has nearly resolved. During the past year, she has had mild abdominal discomfort, which she attributes to menstrual cramps. She has not noticed any vaginal discharge and reports no gastrointestinal or urinary tract symptoms.
The patient is otherwise healthy, with no history of HIV infection, arthritis, or any other comorbidity. She has been sexually active with three partners during the past year and had a miscarriage 6 months ago. She reports that she has used condoms inconsistently during sexual intercourse and is currently taking an oral contraceptive. She has not seen her obstetrician/gynecologist since her miscarriage 6 months earlier.
She reports that she does not have history of substance abuse, including intravenous drug use, but does drink a few beers two or three times per week. She does not smoke, and her body mass index is within normal limits. She has no family history of a similar presentation.
Physical examination and workup
Upon examination, the patient is febrile, with a temperature of 102.6° F (39.2° C). She has a blood pressure of 110/70 mm Hg, a heart rate of 115 beats/min, a respiration rate of 20 breaths/min, and an oxygen saturation of 96%.
Her right shoulder and left wrist joints are painful. No joint erythema is noted, but she has limited range of motion secondary to the pain. She appears to be in severe discomfort.
She has a rash on her body, including on the palms and soles, which has nearly resolved. Residual petechial macules and papules are visible on her wrist. Figure 1 shows a similar rash in a different patient. Similar lesions are noted on the bilateral thighs and perineum, but the degree of involvement is significantly less than it was 2 weeks earlier, according to the patient. The remainder of the physical examination results are unremarkable.
Figure 1:

A urine pregnancy test is negative. Routine laboratory studies are performed. A complete blood cell count reveals a white blood cell count of 9000 cells/µL (reference range, 4000-11,000 cells/µL), with predominantly elevated neutrophils. The urinalysis results are normal. The results of a comprehensive metabolic panel are within normal limits. A rapid plasma reagin test, hepatitis B and C tests, HIV antigen/antibody test, and urine Neisseria gonorrhoeae/Chlamydia trachomatis nucleic acid amplification tests are ordered. Because of the patient’s unusual presentation, blood and urine cultures are also ordered.
Ultrasonography of her right upper quadrant does not show any signs of cholecystitis or cholelithiasis. Contrast CT of her abdomen and pelvis does not reveal hepatic inflammation or any fluid collections.
Gynecology is consulted, and speculum examination is negative for vulvovaginitis, cervicitis, or foreign body. Urine and serum beta human chorionic gonadotropin test results are negative for pregnancy. Physical examination does not reveal cervical or adnexal tenderness or mass. Additional testing includes pap smear, urine nucleic acid amplification test for chlamydia and gonorrhea, human papillomavirus polymerase chain reaction test, and bacterial and fungal cultures. Results are pending.
Transvaginal ultrasonography is performed and does not reveal endometritis, salpingitis, tubo-ovarian abscess, ectopic pregnancy, hydrosalpinx, nor pyosalpinx. Some tubal scarring is noted bilaterally; however, the tubes are not disfigured. Contrast CT of the abdomen and pelvis shows increased perihepatic enhancement that is concerning for perihepatitis and minimal bilateral tubal scarring. The CT is negative for pyosalpinx, tubo-ovarian abscesses, and abdominal or pelvic abscesses. An erect posteroanterior chest radiograph is urgently obtained (Figure 1). An abnormality on the chest radiograph prompts CT of the chest (Figure 2) and the abdomen (not pictured).
On the basis of only these findings, which is the most likely diagnosis?
- Viral hepatitis
- Acute cholecystitis
- Fitz-Hugh-Curtis syndrome
- Amebic liver abscess
Ready to see the answer?
The correct diagnosis is Fitz-Hugh-Curtis syndrome. See the breakdown below.
Fitz-Hugh-Curtis syndrome is a rare manifestation of chronic pelvic inflammatory disease (PID) in young women of childbearing age. The syndrome may mimic numerous other diseases, including:
- Viral hepatitis
- Acute cholecystitis
- Subphrenic or hepatic abscess
- Ectopic pregnancy
- Right-sided renal colic or pyelonephritis
- Pleurisy
- Herpes zoster
- Appendicitis with an atypical presentation
The findings in this patient were specific for Fitz-Hugh-Curtis syndrome. The other options in the differential diagnosis could be excluded on the basis of the clinical presentation and the laboratory results.
This patient has risk factors for the acquisition of viral hepatitis (sex with multiple partners, inconsistent use of contraceptives), and she presents with right upper quadrant pain. However, she does not have jaundice or an acute elevation in aminotransferase levels. In addition, the results of her hepatitis serology tests are negative. Ultrasound and CT imaging do not reveal any hepatic inflammation. These findings make acute viral hepatitis highly unlikely.
Right upper quadrant pain in a woman of childbearing age could be due to acute cholecystitis. The normal liver function results, including alkaline phosphatase, and the absence of evidence of cholelithiasis or cholecystitis on the patient’s right upper quadrant ultrasound rule out this possibility.
Amebic liver abscess can present with a similar clinical scenario; however, the complete blood cell count did not reveal any elevation in eosinophils. Moreover, the hepatic ultrasound and the abdominal CT did not show any fluid collection indicating a hepatic abscess. On the basis of CT findings, gastrointestinal surgery was consulted. Laparoscopy was performed and dense violin string adhesions between the liver and the diaphragm anterior abdominal wall were identified. Figure 2 shows perihepatic adhesions in a different patient. No peritoneal seeding was noted. A KTP/532 laser was introduced through a secondary site, and the adhesions were carefully removed.
Figure 2: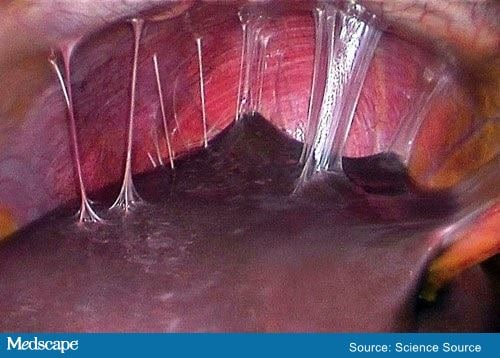
More details
- For the original story and more information about this condition: A Sexually Active 30-Year-Old Woman With Rash and Wrist Pain
- All content for this article belongs to Medscape © 2021 WebMD, LLC. For more case examples, visit Medscape Case Challenges.
- Author: Amber M. Bokhari, MD
Do you have a case you are struggling to diagnose? Or a really unusual case you diagnosed successfully? Share your odd cases with Medical Forum at karl@mforum.com.au.

