By Dr Angamuthu Arun, Gynaecologist, Waikiki
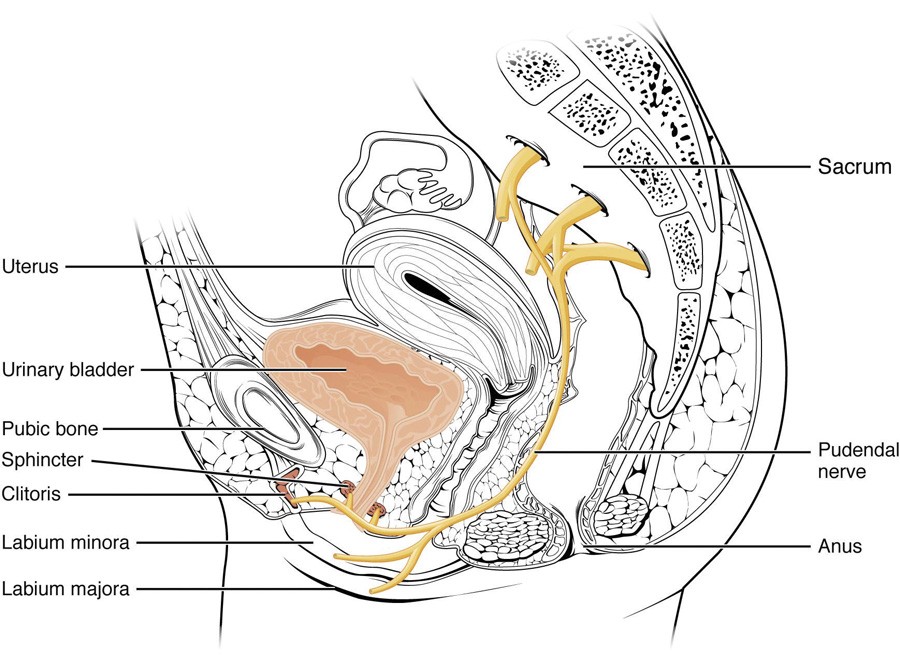
Pudendal neuralgia (prevalence unknown) is long-term pelvic pain that originates from damage to or irritation of the pudendal nerve, one of the main nerves in the pelvis. The nerve supplies areas such as the lower buttocks, the area between the buttocks and genitals (perineum) the area around the back passage (rectum),vulva, labia, and clitoris in women (scrotum and penis in men). (Fig.1). Pudendal neuralgia pain affects more women (60%) than men. The problem is commonly misdiagnosed.

The difference in pudendal neuralgia symptoms
The main symptom is pelvic pain affecting any of the areas supplied by the pudendal nerve.
Pain characteristics may:
- feel like a burning, crushing, shooting or prickling sensation,
- develop gradually or suddenly,
- be constant or fluctuate,
- be worse on sitting and better when standing or lying,
Other symptoms can include:
- numbness and pins and needles in the pelvic area,
- increased sensitivity – just a light touch or wearing clothes can be uncomfortable,
- feeling as though there’s swelling or an object in the perineum (“like a golf or tennis ball”),
- frequency or urgency,
- pain during sex, difficulty reaching orgasm, and erectile dysfunction in men.
Possible causes of pudendal neuralgia
These include:
- compression by nearby muscles or tissues (pudendal nerve entrapment or Alcock canal syndrome)
- prolonged sitting, cycling, horse riding or constipation causing repeated minor damage to the pelvic area
- previous surgery to the pelvic area
- pelvic fractures
- damage to the nerve during childbirth
- a tumour pressing on the pudendal nerve
Diagnosis using Nantes critea
Five of these criteria are required for diagnosis:
- Pain in the anatomical territory of the pudendal nerve;
- Pain aggravated by sitting;
- No nocturnal waking due to pain;
- There is no objective sensory loss on examination;
- A positive response to anaesthetic block of the pudendal nerve.
Other symptoms can also suggest pudendal neuralgia, such as sexual dysfunction, defaecation difficulty and/or urinary symptoms.
Management depends on the cause
Physical therapy has been considered the first-line treatment by many investigators. The management of pudendal neuralgia also includes behavioural modifications, pelvic floor physiotherapy, analgesics, pudendal nerve block, injections of botulinum toxin A (in case of muscle spasms).
Pharmacological treatment varies. Some of the more common medications are gabapentin, pregabalin, cyclobenzaprine, and tricyclic antidepressants. Local medications, such as intravaginal diazepam have also been applied.
Nerve block or surgical decompression can be considered if conservative treatment fails.
Pudendal block. The pudendal nerve carries sensations to and from the vagina, part of the buttocks and the skin between the genitals and the back passage. A pudendal nerve block of local anaesthetic and steroid medication is often done to temporarily reduce pain and aid diagnosis.
In a recent study by Antolak et al, where 52 men received a therapeutic pudendal block in a Minnesota Urology Pain Clinic, local anaesthesia affected all 6 pudendal nerve branches in only 13.2% of patients and complete pain relief occurred in 39.2%.
Surgical decompression is offered when entrapment is suspected and pudendal nerve blocks have provided minimal or no relief. Following this surgery, approximately 40% of patients are pain free, 30% have some improvement in pain, and 30% patients show neither improvement nor worsening.
Key Messages
- Avoid delays in diagnosis and treatment.
- Pudendal neuralgia may be confused with a form of vulvodynia.
- Diagnosis is based on the Nantes criteria.
- Treatments can be conservative (behavioural modification, physiotherapy, analgesics) or not (nerve block, surgical nerve decompression).
Author competing interests: no relevant disclosures.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

