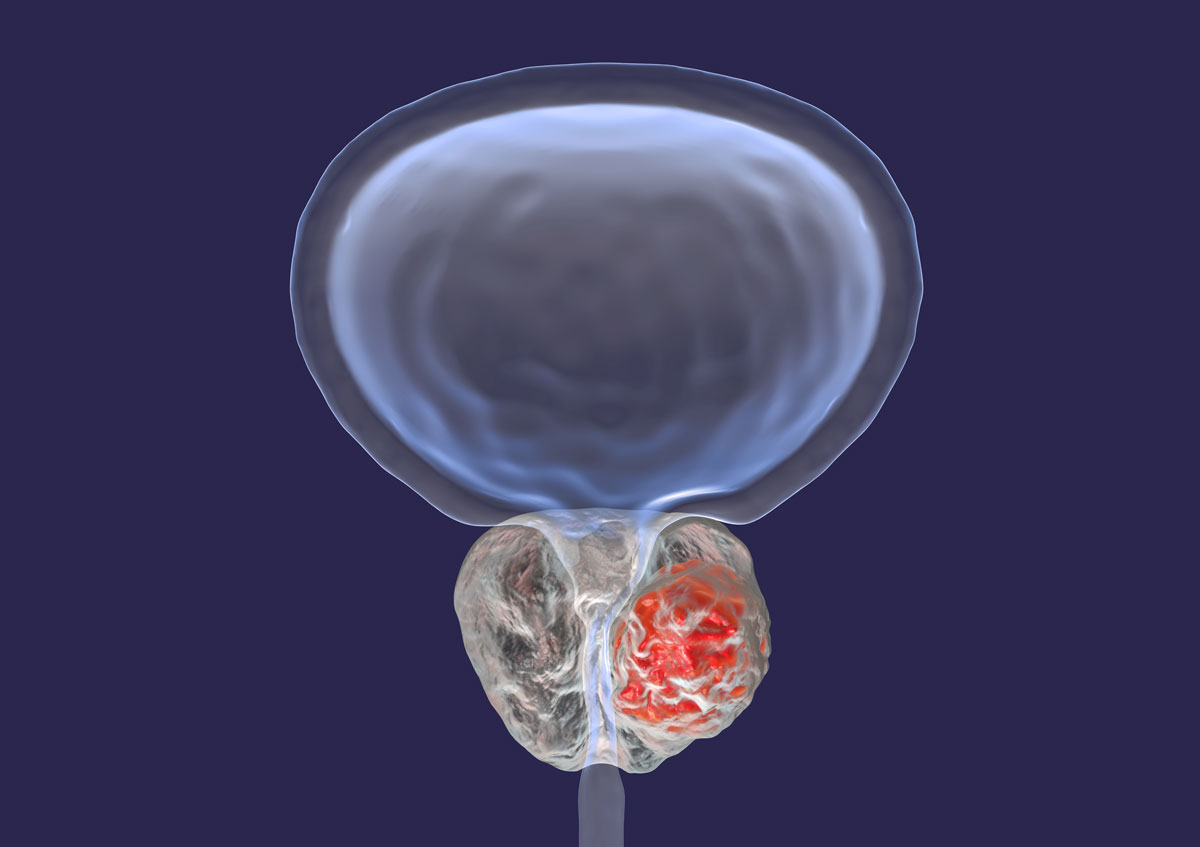
One in seven Australian men will be diagnosed with prostate cancer. Early diagnosis is associated with prolonged survival. With treatment 95% will live at least five years, often 10-20 years. Curative treatment with surgery (radical prostatectomy (RP)) and radiotherapy (RT) is effective but side effects are common and can have major impact on quality of life.
Urinary incontinence (UI) occurs in 5-40%, erectile dysfunction (ED) in up to 80%. Fortunately, effective treatments are available for UI and ED post-treatment. Neither needs to be accepted as inevitable consequences of cancer treatment and quality of life can be restored effectively in most cases. Access to such treatments are hindered by a lack of awareness amongst patients and their GPs.

Urinary incontinence
Any amount of uncontrolled leakage is significant and should be taken seriously. RP results in stress incontinence-leakage occurs in response to ‘stress’ on the bladder (e.g. lifting, coughing, laughing etc, known as SUI). This is due to weakness of the voluntary External Urinary Sphincter (EUS) which resides at the apex of the prostate and suffers direct injury and denervation, particularly in cases of locally advanced cancer where wide resection is necessary.
Radiotherapy can also result in UI but typically this is due to contraction of the bladder with loss of storage capacity in addition to EUS injury and usually develops over a period of years, post-treatment, and can be challenging to manage.
Management options include preoperative weight loss, physiotherapy (pelvic floor muscle strengthening), and anticholinergic medication (not effective in SUI). Surgery is an option where physiotherapy fails. A urethral sling is effective for mild SUI (three pads or under 300ml loss per 24 hours).
An artificial urinary sphincter, which is patient-operated, is 90% effective in severe incontinence. The complication rate (parts failure, infection erosion) is higher than with a sling.
Erectile dysfunction (ED)
This is commonly pre-existing in the those being treated for prostate cancer with 50% at age 50 having some ED, increasing 10% per decade post-surgery most will have severe ED which may improve over 12-36 months. Erectile nerve sparing correlates with recovery but is not always possible with locally advanced or high-grade cancers
ED management can be non-surgical. This includes penile rehabilitation early post-op with PDE5 inhibitors, vacuum device and intracavernosal injections to maintain penile tissue health whilst awaiting nerve function recovery. Penile prostheses may be inflatable (effective with high patient and partner satisfaction). Complications include infection and parts failure. Malleable implants are simpler with less complications but also less effective.
Key messages
- UI and ED are common following prostate cancer treatment and significantly impact quality of life.
- These issues need not be accepted and can be managed effectively.
- Awareness of treatment options is lacking and is key to men accessing care.
References available on request.
Questions? Contact the editor.
Author competing interests: None to disclose.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.