
ED: Dr Catie Thorne from Bunbury gives us the benefit of her experience over bone density reports.
These thoughts on the bone mineral density (BMD) report come after reading the ISCD Official Position Statement 2015, working in General Practice and at the Keogh Institute for Medical Research, and reading reports from different providers.
Some providers issue the BMD report without the scan images. It is worthwhile having them to check quality control, especially if the scan reports a significant change that might change treatment. Inaccurate reports may trigger inappropriate decisions that can be costly and sometimes harmful to patients.
A picture is worth a thousand words. It is very annoying trying to get scan images and it is difficult accessing images due to different reporting “portals” and privacy issues. The graphs help the patient understand the discussion of results.
The same BMD machine should be used each time; a change should be reported, only if it is based on the precision error, and least significant change. A change of serial number or brand of machine may render a reported percentage change insignificant.
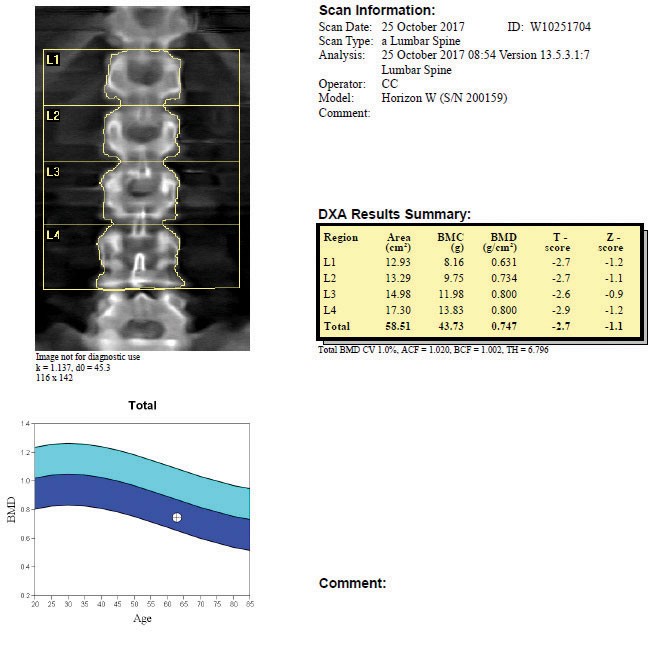 Lumbar spine BMD should be measured using L1-L4, or a minimum of two vertebrae, and checking the same vertebrae are included in subsequent scans. Any artefact should be mentioned and excluded from analysis. Proper consistent positioning of the proximal femur is crucial for the accurate interpretation of femoral neck bone density and, in particular, for any change in hip bone density.
Lumbar spine BMD should be measured using L1-L4, or a minimum of two vertebrae, and checking the same vertebrae are included in subsequent scans. Any artefact should be mentioned and excluded from analysis. Proper consistent positioning of the proximal femur is crucial for the accurate interpretation of femoral neck bone density and, in particular, for any change in hip bone density.
It is not indicated to routinely perform 1/3 radius, as happens in some practices, unless the hip and lumbar spine are not valid, or if the patient’s weight precludes them lying on the densitometer bed.
The diagnosis of osteoporosis or low bone density (osteopaenia) by the T-score is relevant to scans from post menopause or over 50 years, and should be made only on the lumbar spine, femoral neck or total hip. The diagnosis should not be made on the t-score of an individual vertebra or Ward’s triangle. The Z-score (not the T-score) should be used in premenopausal women and those who are under 50 years of age. Statements like “has the bones of an 80-year-old” should never be made.
The online risk calculators (Garvan and FRAX) are developed using the bone density of the femoral neck, not, as some providers do, by choosing the lowest bone density in the scan.
To report risk, previous fragility fracture is important. Bones of the hands and feet or the face are excluded. Some patients incorrectly say they are “minimal trauma facture” for the radiologist, thus erroneously influencing the fracture risk estimate.
The ideal report recognises artefacts, takes into account the recorded history, identifies significant changes since the last scan and perhaps suggests further investigation (e.g. a low Z-score prompts for secondary causes of osteoporosis), and be open to a phone call to question the report.
Author competing interests: nil relevant. Questions? Ask the editor.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

