Achilles tendinopathy is a relatively common condition affecting up to 2% of the population. The cause is usually repetitive intense activity as can be seen in athletes or may also be degenerate in nature. It is most commonly seen in the mid-substance of the Achilles tendon as well as at the insertion into the posterior calcaneum.

The diagnosis can usually be established by clinical examination with focal tenderness and swelling over the mid-substance or swelling at the posterior heel often from an insertional enthesophyte. Pain can be reproduced by tendon loading activity such as a single heel rise. The first priority of clinical examination, however, is to exclude a complete rupture and a calf squeeze test has excellent validity for this.
The main role of imaging is to exclude an associated tear that can alter management and prognosis. Ultrasound scans are useful and colour doppler demonstrates increased blood flow. In a normal Achilles tendon, blood flow is generally not detectable. Abnormal blood flow is linked to greater pain scores, poorer function and prolonged symptoms.
Ultrasound scans have limitations in detecting more proximal partial thickness ruptures closer to the myotendinous junction and differentiating between older partial ruptures and intra-tendinous degeneration. Hence MRI scanning may be more accurate in determining the extent of partial thickness tearing as a percentage of the cross-sectional area of the Achilles tendon.
 Conservative treatments
Conservative treatments
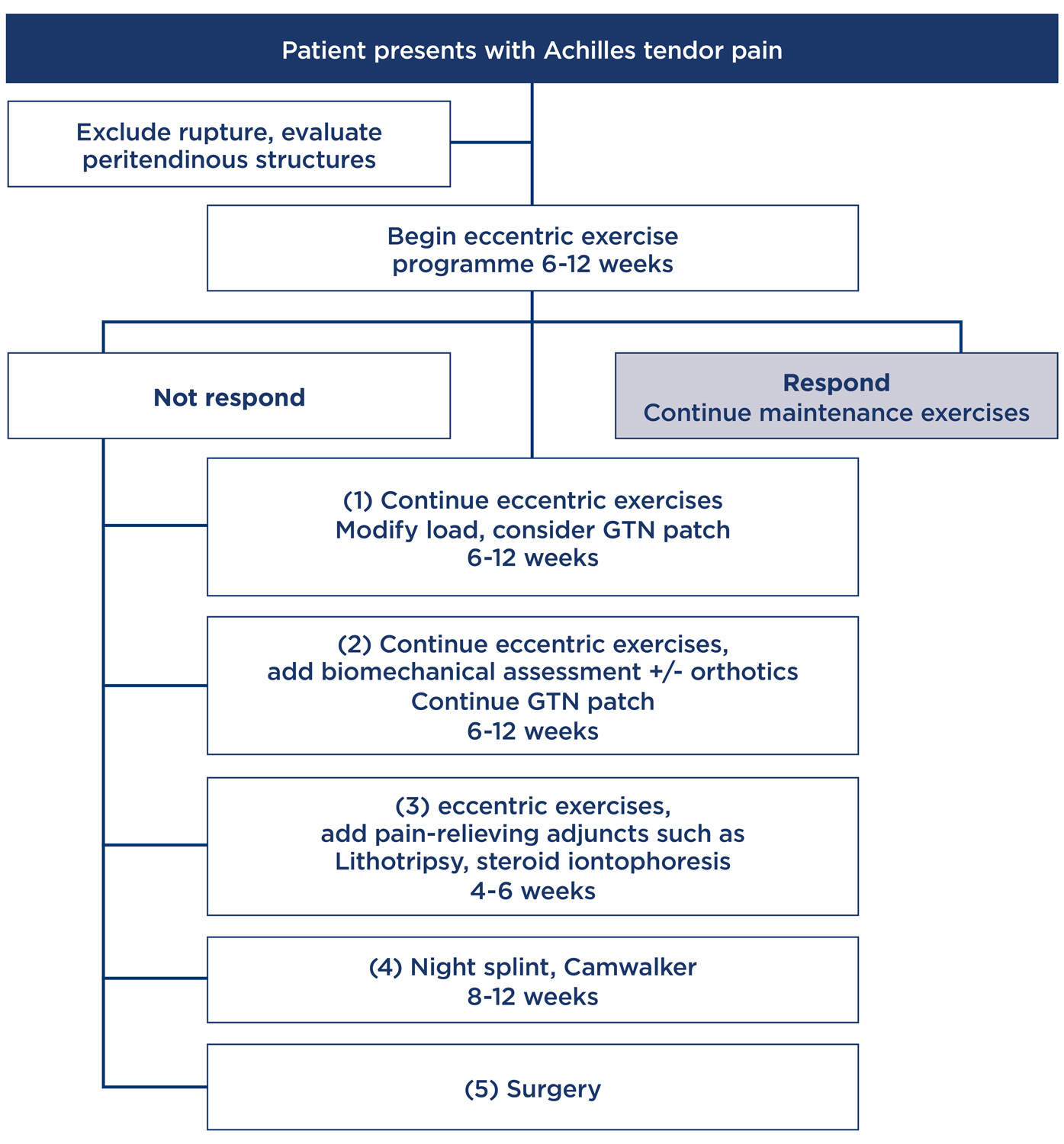
Many treatments are available for chronic Achilles tendinopathy but there is often little scientific evidence for most conservative and surgical treatments. Nevertheless, conservative treatment is recommended as the initial strategy, involving a multifactorial approach including rest and activity modification, and alteration of shoes and orthotics.
Eccentric musculotendinous training exercises lengthen the muscle unit with an external force and alter tendon pathology in the long term with a positive effect on Type 1 collagen production and increasing tendon volume over time, thus increasing tensile strength.
Repetitive stretching and lengthening of the tendon unit may also increase capacity to effectively absorb load. Studies show that a 12-week program of eccentric training can successfully reduce symptoms in approximately 90% of those with mid-substance Achilles tendinopathy, but in only 30% with insertional tendinopathy.
The application of topical Glyceryl Trinitrate directly onto the tendon theoretically helps by increasing local blood supply to stimulate a reparative response, and also through the action of nitric oxide to stimulate collagen and tendon healing. There are potential side-effects of hypotension and headaches, and it is thus best to initially use Glyceryl Trinitrate when sleeping.

Extracorporeal Shockwave Therapy has been shown to reduce pain by probably promoting regenerative processes in the Achilles tendon.
Short-term effects of corticosteroid injections reduce pain and swelling. However intra-tendinous injections are contra-indicated because of the catabolic effects of the steroid which can cause tendon ruptures. Corticosteroids reduce inflammation and inhibit production of granulation tissue and adhesions.
Local corticosteroid injections around the Achilles tendon and associated bursae do have a lower but still significant risk of causing a tendon rupture. As such iontophoresis is perhaps a safer method of delivering corticosteroids.
Night splints have been shown to be an effective intervention to help to stretch the tendon unit and overcome associated gastrocnemius contractures. Immobilisation fully weight-bearing in a Camwalker can have similar effects as well as preventing overload of the tendon during walking.
Surgery
Surgical treatment is indicated for those who fail to respond to conservative treatment. It includes percutaneous or open tenosynovectomies which can result in long-term improvement with 75% of patients reporting good or excellent results after 18 months. More controversial treatments include percutaneous or open tenotomies to stimulate a healing response.
Of more concern is a partial thickness tear which can potentially result in a full thickness tear. This is increased by corticosteroid injections and medications such as Fluoroquinolones. There is also the risk of spontaneous conversion to a complete rupture. Once over 30% of the cross-sectional area has commenced tearing the risk escalates. In these patients’ debridement and Achilles tendon repair can lead to excellent results in terms of pain resolution and preventing complete rupture.
Key messages
- Chronic Achilles tendinopathy is easily treated in general practice.
- Many conservative treatment options can relieve most tendon pain
- Most failing to respond to conservative care will find relief from surgical treatment.
– References available on request
Author competing interests – nil

