Pneumococcal disease and herpes zoster represents considerable health burden both in Australia and globally accounting for 25% and 7% of Disability Adjusted Life Years (DALY) of vaccine preventable disease burden. Between 1997 and 2016, pneumococcal disease resulted in 622 deaths and 2434 hospitalisations.


Older Australians have a greater likelihood of developing both conditions than the general population. The risk of developing complications in both conditions is significantly reduced by vaccination which the National Immunisation Program (NIP) funds for those over 70 years.
This audit reviewed the proportion of patients aged above 70 years (between 1/01/2017 to 30/12/2020) receiving the recommended vaccination against pneumococcal disease and varicella. It was performed in an outer Perth metropolitan general practice, a region that has a higher-than-average rate of vaccine preventable hospitalisation compared to the national average.
Methods
A case was defined as any patient who attended two GP appointments at this medical practice between 1 January 2017 and 31 December 2020, without an additional risk factor for either condition, and turned 70 years in the review period. Exclusion criteria were patients who received a varicella zoster vaccine prior to the data collection period, who received a pneumococcal vaccine prior to the data collection period and those with a contraindication to either vaccine
It was planned that the first 50 randomised patients not meeting the exclusion criteria would be used in this audit, however only 47 participants did not meet the exclusion criteria.
For Medicare eligible persons that attended this medical practice who turned 70 years in the data collection period; 80% patients received a recommendation for a pneumococcal vaccine and a live attenuated varicella zoster vaccine between 1/01/2017 to 30/12/2020.
The benchmark of 80% was chosen as a composite of research demonstrated greater than 70% uptake for both vaccines is standard globally with 10% refusal rate for vaccination. The data was collected from the practice’s patient management software using pre-programmed search parameters for date of birth and visit history. Demographics, medical history, and vaccination data were checked manually. All other GP written patient notes were examined for vaccine recommendation or counselling.
Results
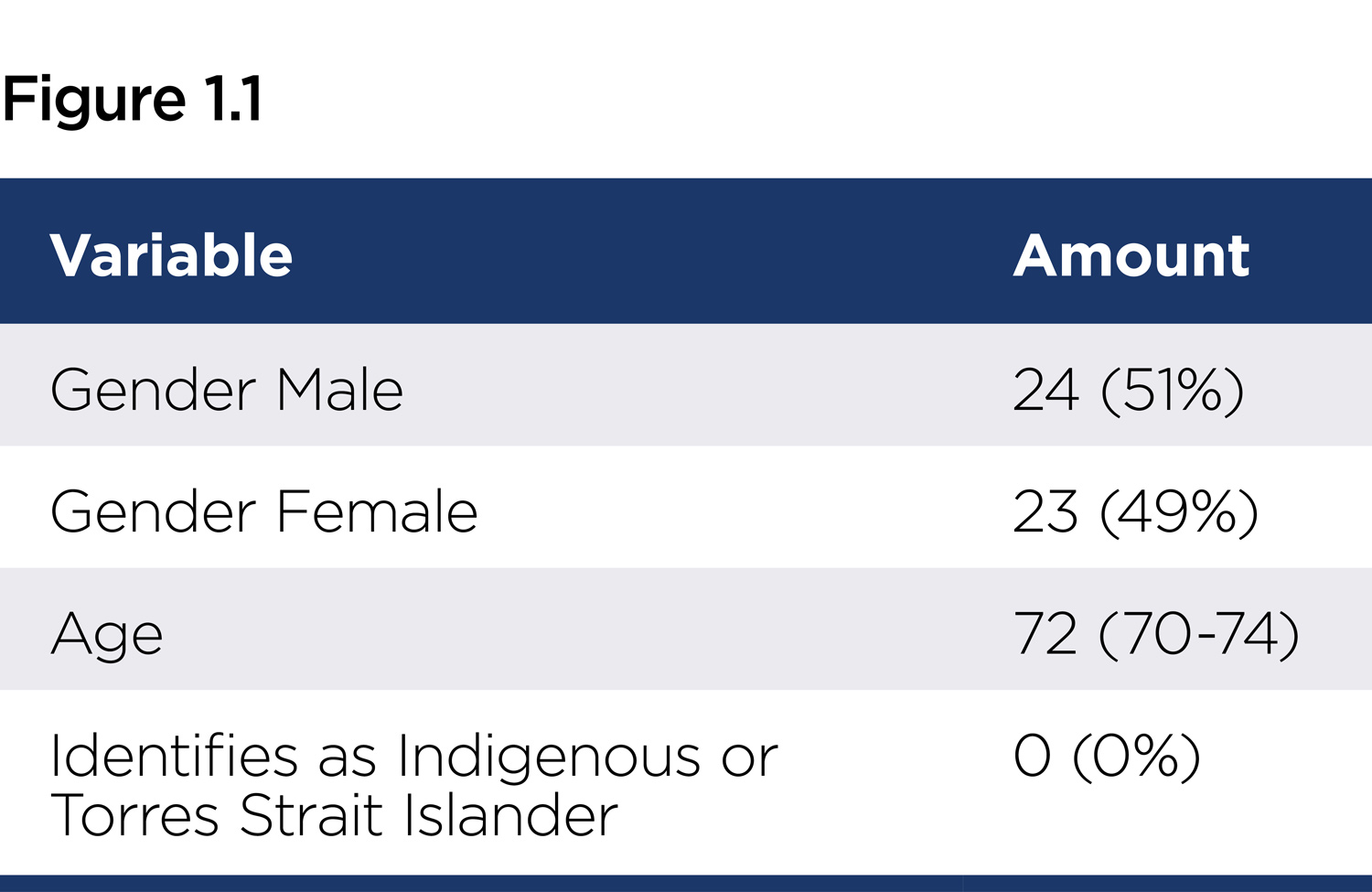 A total of 78 cases were reviewed for this audit; 47 cases were then included in the audit. Demographics are outlined in Figure 1.1, the gender ratio being consistent with regional data.
A total of 78 cases were reviewed for this audit; 47 cases were then included in the audit. Demographics are outlined in Figure 1.1, the gender ratio being consistent with regional data.
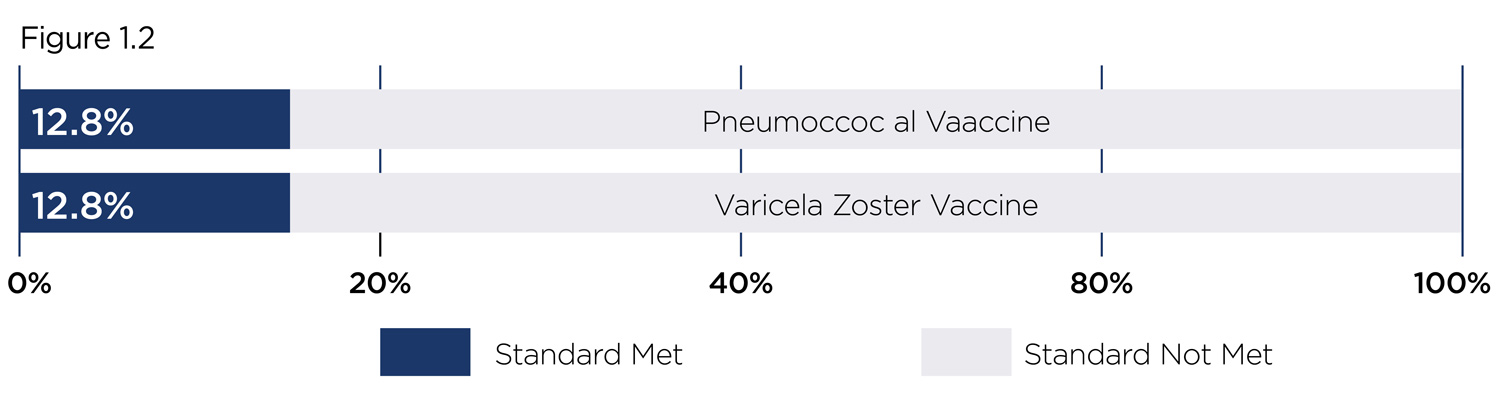
Neither of the standards were met in this audit. Figure 1.2 presents the performance of the practice as a percentage of achieving each standard. Numerically, only six cases had documentation to support that they had received a recommendation or counselling to receive the pneumococcal vaccine, and separately, the varicella zoster vaccination.
The result was unexpected, especially for pneumococcal vaccination rates, due to the nature of awareness around the vaccine and the previous studies showing higher levels of uptake. The varicella zoster vaccination outcome was neither expected nor unexpected, as there were large variations in the reported literature regarding the uptake in the community.
The audit has limitations. Firstly, some GPs stated that due to time constraints, not all preventative health recommendations were documented. Furthermore, due to patients visiting several GPs for their care, it was likely that a patient presenting from another practice did not have an accurate immunisation history at the practice being consulted. Therefore, the true rate of vaccine recommendation is likely higher.
Previous studies have identified barriers to preventative health activities including a medical model focused on curative medicine rather than preventative medicine, ambivalence toward preventative health activities and a lack of clearly defined roles for nurses in general practice in relation to preventative health.
 The audit can cautiously be interpreted as a paucity of patients receiving education or counselling regarding the two vaccines in question, which may be comparable to other similar general practices in Australia. This is significant, as members of this age group are more likely than the general population to suffer adverse health effects related to these two conditions, with associated burden for the Australian healthcare system.
The audit can cautiously be interpreted as a paucity of patients receiving education or counselling regarding the two vaccines in question, which may be comparable to other similar general practices in Australia. This is significant, as members of this age group are more likely than the general population to suffer adverse health effects related to these two conditions, with associated burden for the Australian healthcare system.
Some of the recommendations suggested included an action plan for staff education, dissemination of literature and consideration of reaudit in 12-24 months.
Key messages
- This clinical audit showed that the pneumococcal and varicella vaccine education provided in general practice in patients over 70 years was lower compared to the standards
- This audit highlights the increased need for vaccine education in the over 70s.
– References available on request
ED: Xavier Cornwall is a medical student at the University of Notre Dame, and Dr Raman is a lecturer and supervisor
Author competing interests – nil

