You’re getting older…maybe your heart or lungs aren’t working like they used to. Perhaps your brain is beginning to forget things. As you stride or stumble past 70 life will be become more fragile. If you suffer a significant medical happening – a heart attack, a stroke, a pneumonia – who will make the call as to what treatment we should offer you?
As a palliative care consultant at RPH, I’m regularly seeing elderly patients present to our Emergency Department (ED) with life threatening conditions and the dilemma facing us all is ‘to treat or not to treat’.

In the past with our ‘can do, should do attitude’ we would actively treat all who came our way. Usually this was with the family urging and supporting this approach. The outcomes were mixed.
We could recover many patients but not always to their former baseline. Many would be back in ED a few weeks later in a similar or worse condition. Often for those who survived there would be a significant amount of additional suffering: a diminished functional level, an increased symptom burden, social dislocation.
Our approach is changing
We received a referral from ED to see an elderly lady, in poor general condition, with dementia and recurrent pneumonia. The son desperately hoped his mother would recover with our ‘good’ treatment. While a trial of antibiotics had been started, the ED doctor discussed in a compassionate, considered way that the outlook was poor, and the likely outcome was that his mother would die in the next few days. He completed a Goals of Patient Care (GOPC) form, ticking the ‘Optimal comfort care’ option, which her son accepted.
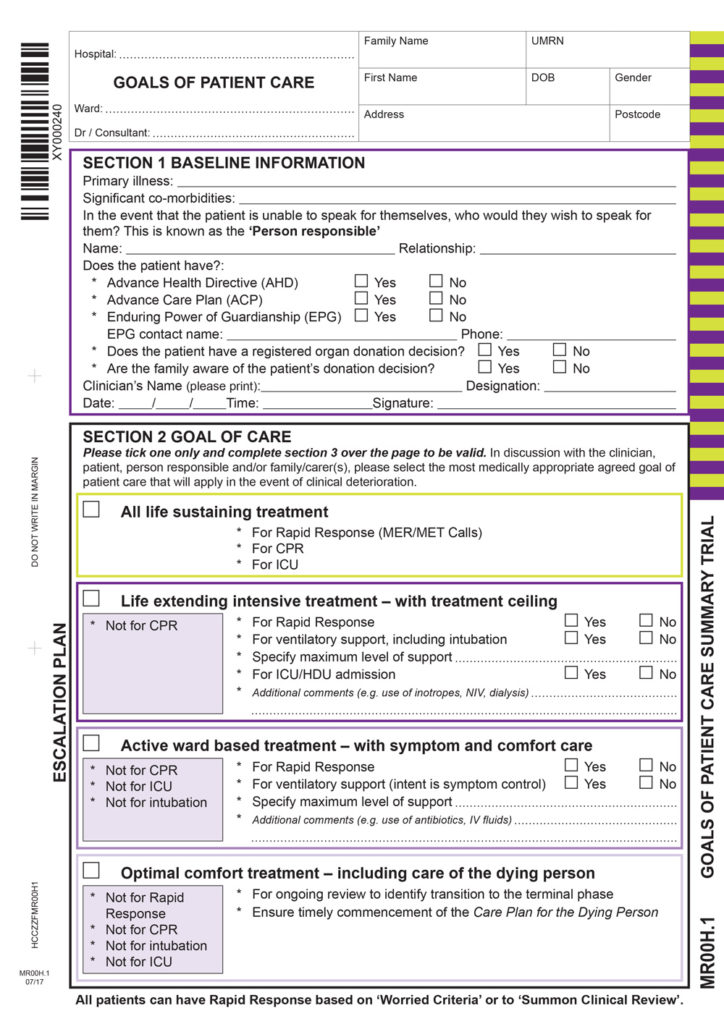
GOPC is a form and a process. We used to complete a ‘Not for Resuscitation’ form for patients we did not think would benefit from CPR or intensive treatments. Now we are getting better at understanding and accepting what are the probabilities of success from our treatments especially with our frail patients. GOPC allows us to discuss these probabilities with our patients and their families and discover what their expectations and care preferences might be.
GOPC is a hospital-driven process trying to match a person’s illness and goals with what the hospital system has to offer. It can be guided by the Advance Health Directive (AHD) or Advance Care Plan (ACP). Do you have one? If not, how will we know how much treatment you may or may not want?
Thankfully more realistic, open, compassionate discussions are happening and making ‘the call’ is becoming less difficult. As we try to best traverse the life-and-death decision zone, clarity, honesty and a compassionate approach are essential travelling aids.
Key messages
- GOPC aims to match a person’s illness and goals with what the hospital system has to offer
- An Advance Health Directive or Advance Care Plan assists hospital teams to complete Goals of Care
- Open, compassionate discussions are making ‘the call’ less difficult.
Questions? Contact the editor.
Author competing interests: Nil.
Disclaimer: Please note, this website is not a substitute for independent professional advice. Nothing contained in this website is intended to be used as medical advice and it is not intended to be used to diagnose, treat, cure or prevent any disease, nor should it be used for therapeutic purposes or as a substitute for your own health professional’s advice. Opinions expressed at this website do not necessarily reflect those of Medical Forum magazine. Medical Forum makes no warranties about any of the content of this website, nor any representations or undertakings about any content of any other website referred to, or accessible, through this website.

