Cardiovascular disease is the leading cause of morbidity and mortality worldwide. Coronary artery disease is the most common type of cardiovascular disease. Aortic dissection and pulmonary embolism are the other two common forms presenting the symptom of acute chest pain similar to that of coronary artery disease, as observed in the Emergency Department.

Imaging diagnosis plays an essential role in the early detection of cardiovascular disease, with an intense focus on the characterisation of lesions and identifying vulnerable patients to guide timely treatment and avoid adverse cardiac events.
Cardiac computed tomography (CT) is the most commonly used imaging modality in diagnosing and assessing cardiovascular disease due to its wide availability and rapid technological improvements in scanning techniques with a high diagnostic value. Importantly, cardiac CT serves as the first-line technique to diagnose and screen patients with cardiovascular disease, thus, avoiding unnecessary invasive procedures and reducing costs or complications.
One limitation of cardiac CT imaging at present is the high radiation dose, which might be a concern in the current medical practice. Another limitation of CT imaging (along with other imaging modalities) is the lack of ability to demonstrate complex anatomy and pathology in real-time three-dimensional (3D) view, despite the capability of reconstructing the volume data into 2D and 3D views. This drawback can be overcome by the increasing applications of 3D printing technology in the medical domain.
The CVD context
3D printing was developed in the early 1980s. However, the recent surge in its use is due to technological advancements and its increasing applications in the medical field. This approach reduces the turnaround time to printing physical models and the associated cost of printing materials. The personalised 3D printed models based on medical imaging datasets, such as cardiac CT images, have significant value in cardiovascular disease.
The applications range from improving the understanding of complex cardiovascular anatomy and pathology (especially congenital heart disease) to pre-surgical planning and simulation of challenging cardiac procedures, enhancing the education of medical students or healthcare professionals and doctor-patient communication.
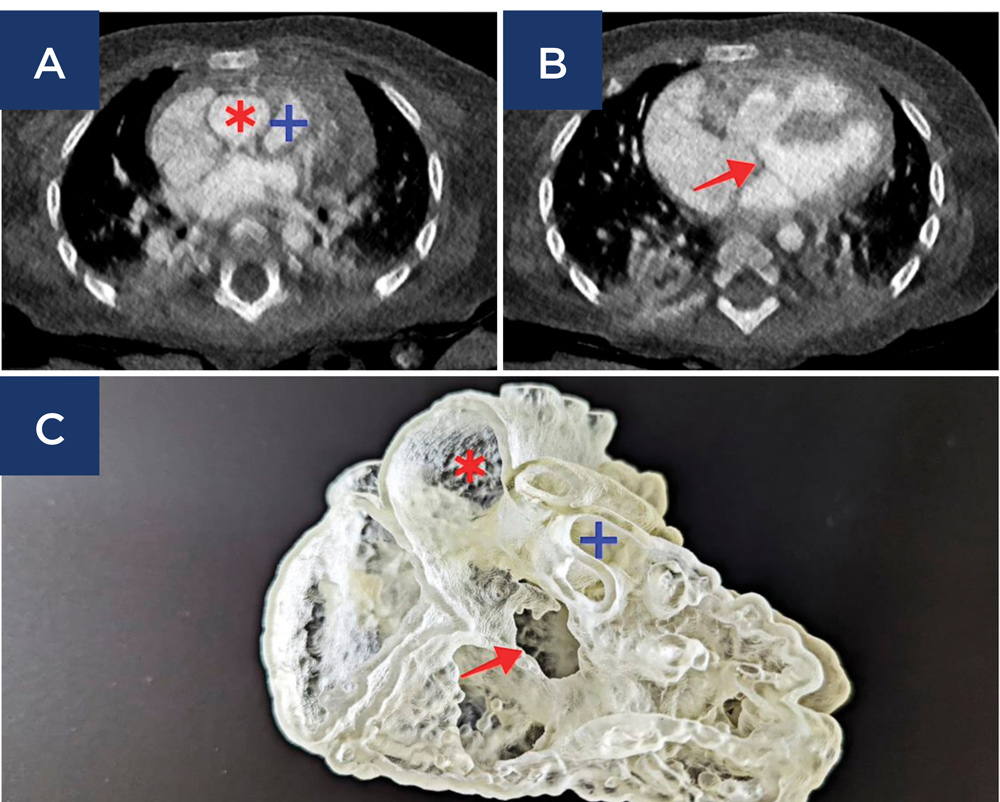
A: Cardiac CT image shows the rightward displacement of the aorta in the case of DORV with aorta arising from right ventricle;
B: Cardiac CT image shows the ventricular septal defect in DORV;
C: 3D printed model of the case of DORV demonstrates both aorta and pulmonary trunk arising from the right ventricle. Red asterisk * = aorta; blue cross + = pulmonary trunk; red arrow = ventricular septal defect.
Both multicentre and single-centre studies have shown that 3D printed heart models help the surgeons to define the best approach before surgery, thus achieving a personalised therapeutic strategy for each patient. Several randomised controlled trials have confirmed the advantages of 3D printed models over traditional teaching methods in the area of complex congenital heart disease.
An emerging interest in 3D printing in cardiovascular disease is its clinical value in enhancing doctor-patient communication in daily practice.
A scenario in a busy clinical environment exhibits the potential value of how 3D printed models can transform our practice by enhancing doctor-patient communication and equipping doctors with more time to focus on the surgery.
A paediatric patient with suspected congenital heart disease was admitted under a cardiologist. After checking the patient’s history and physical examination, the cardiologist refers the patient to undergo a cardiac CT scan that reveals the presence of a double outlet right ventricle (DORV) (Figure 1A and 1B).
Given the complexity of the congenital anomaly of this disease, cardiac CT images are post-processed by an experienced radiographer on a CT workstation with a segmented volume data file sent to an onsite 3D printer for printing the physical model of this case.
After 24 hours, a personalised 3D printed heart model (Figure 1C) was created, and the cardiologist presented it to the parents of the patient, explaining the condition and the extent of the disease. Then, the patient is referred to a paediatric cardiac surgeon for planning the surgical treatment.
Subsequently, the patient’s parents have a good understanding of their child’s condition while junior doctors can practise the operational procedures on the model for training, and the surgeons plan treatment approaches to minimise the risks or complications. This phenomenon would be expected soon in clinical practice, with the incorporation of 3D printing technology into routine diagnostic strategy and clinical decision-making.
Key messages
- 3D printing has significant value in cardiovascular disease by replicating the complexity of anatomy and pathology
- Personalised 3D printed models assist surgical planning and treatment options.
- 3D printed physical models enhance doctor-patient communication in a busy clinical environment.
Author competing interests – nil

