A roadmap for the Western Australian health system has been outlined in the WA Health Digital Strategy 2020-2030 and features a plethora of initiatives planned for not only the system, but also clinicians, and ultimately, health consumers.
A roadmap for the Western Australian health system has been outlined in the WA Health Digital Strategy 2020-2030 and features a plethora of initiatives planned for not only the system, but also clinicians, and ultimately, health consumers.
The impetus for the strategy came from the final report of the Sustainable Health Review, which was published in April, 2019. The report recommended a long-term digital strategy including a 10-year digitisation plan.
According to Judith Stewart, Executive Director of Strategy, Policy and Planning at the WA Department of Health, the strategy follows on from the digitisation plan and a “vision for how to use innovation and technology to transform the health services and the way that they deliver care over the next decade.”

The strategy has been developed with a clearly defined person-centred focus to ensure the outcomes are beneficial for the end-users by including them in the development and implementation of the proposed initiatives, Judith told Medical Forum.
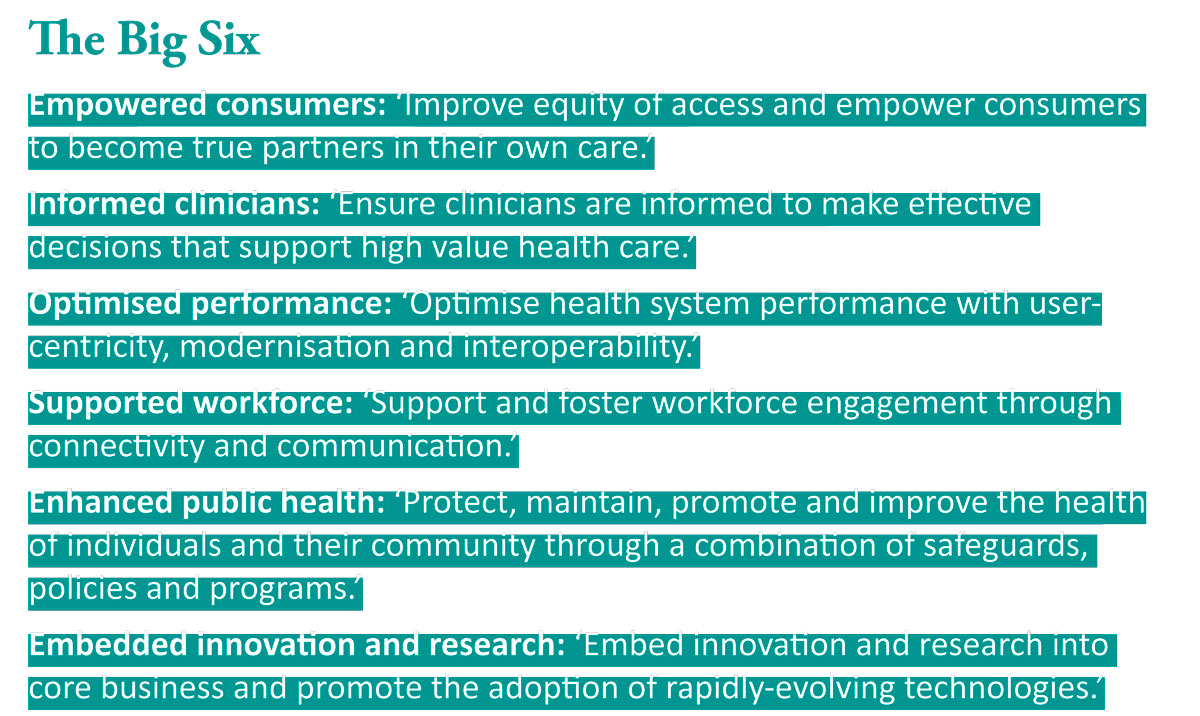
The person-centred approach encompasses six key areas of focus to be integrated into all aspects of the strategy: empowered consumers; informed clinicians; optimised performance; supported workforce; enhanced public health; and embedded innovation and research.
Crucial to the strategy’s success, says Judith, is a unified electronic medical record (EMR) for WA Health and it is currently in the early stages of mobilisation. The EMR will be bespoke to WA with the intention of interoperability with My Health Record.
In the cloud
Implementation will take place in four distinct phases, with Judith emphasising the importance of the first, foundation phase, which will focus on modernising and increasing the capability of the information and communication infrastructure, as part of the HealthNext project. In essence, a migration from physical to cloud-based infrastructure.
While the strategy can be read as a document long on ambitious objectives, and possibly alienate those with interest or aptitude in technology, by it taking a person-centred approach, the end-user’s digital capability is a priority across the board, Judith said.
“We have some great expertise in clinical execution, but we need to make sure that all of our staff are supported and enabled to provide modern, digital care, so we need to have an understanding of what their digital capabilities are, and consulting with those key clinical groups,” she said.
Forward planning for digital innovation can be undone by the advancement of the technology itself. What could be considered fit-for-purpose and future-proof could also be redundant before it is even implemented, so it will require flexibility to adapt.
Judith said the strategy has been designed with that flexibility in mind, particularly beyond the first phase.
“When we undertake a horizon scan and assessment, we need to ensure that those initiatives can adopt transformational change that may be ready for that initiative,” she said.
Successful implementation of the proposed strategies, such as the EMR, will be dependent on the malleability of the infrastructure and the usability of the interfaces, as the end-users need to be able to experience the benefits of adopting the new systems.
“The people that really make the difference are the ones who adopt and use these systems. We need to ensure that we are constantly in dialogue with them and we have the right feedback mechanisms to understand what the clinicians and the users on the ground are experiencing, so that we can be agile and adaptable,” she said.
“Our measures of success will be what are our stakeholders are feeling and experiencing about their delivered outcomes. It has to be something that is at the forefront of our minds as we as we move through implementation.”
Artificial intelligence (AI) and machine learning are rapidly advancing in clinical applications, especially imaging, yet one area where this technology could be revolutionary is in predictive informatics, which Judith highlights as an area of interest.
Being clever with AI
“There is evidence to show that predictive and analytical capability not only changes some of the dimensions of care but also helps predict demand capacity. This is really meaningful where it can transform clinical care – when AI intervenes and predicts patient outcomes earlier, such as patient deterioration. This could allow our clinicians to respond sooner than they do currently.
“It’s our intention to take further advantage of automation and robotics, which we already use, such as TeleHealth, considering how we can use some of these existing tools differently, not just in WA Health but across the whole health ecosphere. That could lead us to looking at opportunities in aged care, for example, using Telehealth for consultations, which could be more convenient for the patient rather than from a purely clinical perspective.”
“We have this great opportunity to work meaningfully with clinicians on the ground, capitalise on some of those fantastic projects around capability already underway, and to discuss with consumers how technology can deliver for them. Ultimately, to do something useful that is tailored for WA and that meets our unique needs.”